General Information About Pituitary Tumors
A pituitary tumor is a growth of abnormal cells in the tissues of the pituitary gland.
Pituitary tumors form in the pituitary gland, a pea-sized organ in the center of the brain, just above the back of the nose. The pituitary gland is sometimes called the "master endocrine gland" because it makes hormones that affect the way many parts of the body work. It also controls hormones made by many other glands in the body.
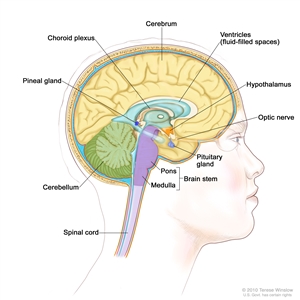
Anatomy of the inside of the brain, showing the pineal and pituitary glands, optic nerve, ventricles (with cerebrospinal fluid shown in blue), and other parts of the brain.
Pituitary tumors are divided into three groups:
- Benign pituitary adenomas: Tumors that are not cancer. These tumors grow very slowly and do not spread from the pituitary gland to other parts of the body.
- Invasive pituitary adenomas: Benign tumors that may spread to bones of the skull or the sinus cavity below the pituitary gland.
- Pituitary carcinomas: Tumors that are malignant (cancer). These pituitary tumors spread into other areas of the central nervous system (brain and spinal cord) or outside of the central nervous system. Very few pituitary tumors are malignant.
Pituitary tumors may be either non-functioning or functioning.
- Non-functioning pituitary tumors do not make extra amounts of hormones.
- Functioning pituitary tumors make more than the normal amount of one or more hormones. Most pituitary tumors are functioning tumors. The extra hormones made by pituitary tumors may cause certain signs or symptoms of disease.
The pituitary gland hormones control many other glands in the body.
Hormones made by the pituitary gland include:
- Prolactin: A hormone that causes a woman's breasts to make milk during and after pregnancy.
- Adrenocorticotropic hormone (ACTH): A hormone that causes the adrenal glands to make a hormone called cortisol. Cortisol helps control the use of sugar, protein, and fats in the body and helps the body deal with stress.
- Growth hormone: A hormone that helps control body growth and the use of sugar and fat in the body. Growth hormone is also called somatotropin.
- Thyroid-stimulating hormone: A hormone that causes the thyroid gland to make other hormones that control growth, body temperature, and heart rate. Thyroid-stimulating hormone is also called thyrotropin.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): Hormones that control the menstrual cycle in women and the making of sperm in men.
Having certain genetic conditions increases the risk of developing a pituitary tumor.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn't mean that you will not get cancer. Talk with your doctor if you think you may be at risk. Risk factors for pituitary tumors include having the following hereditary diseases:
- Multiple endocrine neoplasia type 1 (MEN1) syndrome.
- Carney complex.
- Isolated familial acromegaly.
Signs of a pituitary tumor include problems with vision and certain physical changes.
Signs and symptoms can be caused by the growth of the tumor and/or by hormones the tumor makes or by other conditions. Some tumors may not cause signs or symptoms. Check with your doctor if you have any of these problems.
Signs and symptoms of a non-functioning pituitary tumor
Sometimes, a pituitary tumor may press on or damage parts of the pituitary gland, causing it to stop making one or more hormones. Too little of a certain hormone will affect the work of the gland or organ that the hormone controls. The following signs and symptoms may occur:
- Headache.
- Some loss of vision.
- Loss of body hair.
- In women, less frequent or no menstrual periods or no milk from the breasts.
- In men, loss of facial hair, growth of breast tissue, and impotence.
- In women and men, lower sex drive.
- In children, slowed growth and sexual development.
Most of the tumors that make LH and FSH do not make enough extra hormone to cause signs and symptoms. These tumors are considered to be non-functioning tumors.
Signs and symptoms of a functioning pituitary tumor
When a functioning pituitary tumor makes extra hormones, the signs and symptoms will depend on the type of hormone being made.
Too much prolactin may cause:
- Headache.
- Some loss of vision.
- Less frequent or no menstrual periods or menstrual periods with a very light flow.
- Trouble becoming pregnant or an inability to become pregnant.
- Impotence in men.
- Lower sex drive.
- Flow of breast milk in a woman who is not pregnant or breast-feeding.
Too much ACTH may cause:
- Headache.
- Some loss of vision.
- Weight gain in the face, neck, and trunk of the body, and thin arms and legs.
- A lump of fat on the back of the neck.
- Thin skin that may have purple or pink stretch marks on the chest or abdomen.
- Easy bruising.
- Growth of fine hair on the face, upper back, or arms.
- Bones that break easily.
- Anxiety, irritability, and depression.
Too much growth hormone may cause:
- Headache.
- Some loss of vision.
- In adults, acromegaly (growth of the bones in the face, hands, and feet). In children, the whole body may grow much taller and larger than normal.
- Tingling or numbness in the hands and fingers.
- Snoring or pauses in breathing during sleep.
- Joint pain.
- Sweating more than usual.
- Dysmorphophobia (extreme dislike of or concern about one or more parts of the body).
Too much thyroid-stimulating hormone may cause:
- Irregular heartbeat.
- Shakiness.
- Weight loss.
- Trouble sleeping.
- Frequent bowel movements.
- Sweating.
Other general signs and symptoms of pituitary tumors:
- Nausea and vomiting.
- Confusion.
- Dizziness.
- Seizures.
- Runny or "drippy" nose (cerebrospinal fluid that surrounds the brain and spinal cord leaks into the nose).
Imaging studies and tests that examine the blood and urine are used to detect (find) and diagnose a pituitary tumor.
The following tests and procedures may be used:
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) depends on the type of tumor and whether the tumor has spread into other areas of the central nervous system (brain and spinal cord) or outside of the central nervous system to other parts of the body.
Treatment options depend on the following:
- The type and size of the tumor.
- Whether the tumor is making hormones.
- Whether the tumor is causing problems with vision or other signs or symptoms.
- Whether the tumor has spread into the brain around the pituitary gland or to other parts of the body.
- Whether the tumor has just been diagnosed or has recurred (come back).
Stages of Pituitary Tumors
Once a pituitary tumor has been diagnosed, tests are done to find out if it has spread within the central nervous system (brain and spinal cord) or to other parts of the body.
The extent or spread of cancer is usually described as stages. There is no standard staging system for pituitary tumors. Once a pituitary tumor is found, tests are done to find out if the tumor has spread into the brain or to other parts of the body. The following test may be used:
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Pituitary tumors are described in several ways.

Pea, peanut, walnut, and lime show tumor sizes.
Pituitary tumors are described by their size and grade, whether or not they make extra hormones, and whether the tumor has spread to other parts of the body.
The following sizes are used:
- Microadenoma: The tumor is smaller than 1 centimeter.
- Macroadenoma: The tumor is 1 centimeter or larger.
Most pituitary adenomas are microadenomas.
The grade of a pituitary tumor is based on how far it has grown into the surrounding area of the brain, including the sella (the bone at the base of the skull, where the pituitary gland sits).
Recurrent Pituitary Tumors
A recurrent pituitary tumor is cancer that has recurred (come back) after it has been treated. The cancer may come back in the pituitary gland or in other parts of the body.
Treatment Option Overview
There are different types of treatment for patients with pituitary tumors.
Different types of treatments are available for patients with pituitary tumors. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Four types of standard treatment are used:
Surgery
Many pituitary tumors can be removed by surgery using one of the following operations:
- Transsphenoidal surgery: A type of surgery in which the instruments are inserted into part of the brain by going through an incision (cut) made under the upper lip or at the bottom of the nose between the nostrils and then through the sphenoid bone (a butterfly-shaped bone at the base of the skull) to reach the pituitary gland. The pituitary gland lies just above the sphenoid bone.
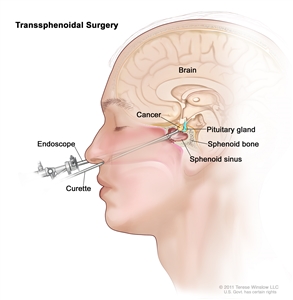
Transsphenoidal surgery. An endoscope and a curette are inserted through the nose and sphenoid sinus to remove cancer from the pituitary gland. - Endoscopic transsphenoidal surgery: A type of surgery in which an endoscope is inserted through an incision (cut) made at the back of the inside of the nose and then through the sphenoid bone to reach the pituitary gland. An endoscope is a thin, tube-like instrument with a light, a lens for viewing, and a tool for removing tumor tissue.
- Craniotomy: Surgery to remove the tumor through an opening made in the skull.
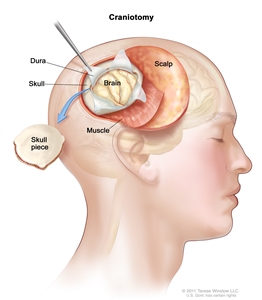
Craniotomy: An opening is made in the skull and a piece of the skull is removed to show part of the brain.
Even if the doctor removes all the cancer that can be seen at the time of the surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer. Certain ways of giving radiation therapy can help keep radiation from damaging nearby healthy tissue. This type of radiation therapy may include the following:
- Stereotactic radiosurgery: A rigid head frame is attached to the skull to keep the head still during the radiation treatment. A machine aims a single large dose of radiation directly at the tumor. This procedure does not involve surgery. It is also called stereotaxic radiosurgery, radiosurgery, and radiation surgery.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type of the cancer being treated. External radiation therapy is used to treat pituitary tumors.
Drug therapy
Drugs may be given to stop a functioning pituitary tumor from making too many hormones.
Chemotherapy
Chemotherapy may be used as palliative treatment for pituitary carcinomas, to relieve symptoms and improve the patient's quality of life. Chemotherapy uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type of the cancer being treated.
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. See the Treatment Options section that follows for links to current treatment clinical trials. These have been retrieved from NCI's listing of clinical trials.
Follow-up tests may be needed.
Some of the tests that were done to diagnose the cancer or to find out the stage of the cancer may be repeated. Some tests will be repeated in order to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Treatment Options for Pituitary Tumors
Non-functioning Pituitary Tumors
Treatment may include the following:
- Surgery (transsphenoidal surgery, if possible) to remove the tumor, followed by watchful waiting (closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change). Radiation therapy is given if the tumor comes back.
- Radiation therapy alone.
Treatment for luteinizing hormone -producing and follicle-stimulating hormone -producing tumors is usually transsphenoidal surgery to remove the tumor.
Prolactin-Producing Pituitary Tumors
Treatment may include the following:
- Drug therapy to stop the tumor from making prolactin and to stop the tumor from growing.
- Surgery to remove the tumor (transsphenoidal surgery or craniotomy) when the tumor does not respond to drug therapy or when the patient cannot take the drug.
- Radiation therapy.
- Surgery followed by radiation therapy.
ACTH-Producing Pituitary Tumors
Treatment may include the following:
- Surgery (usually transsphenoidal surgery) to remove the tumor, with or without radiation therapy.
- Radiation therapy alone.
- Drug therapy to stop the tumor from making ACTH.
- A clinical trial of stereotactic radiation surgery.
Growth Hormone-Producing Pituitary Tumors
Treatment may include the following:
- Surgery (usually transsphenoidal or endoscopic transsphenoidal surgery) to remove the tumor, with or without radiation therapy.
- Drug therapy to stop the tumor from making growth hormone.
Thyroid-Stimulating Hormone-Producing Tumors
Treatment may include the following:
- Surgery (usually transsphenoidal surgery) to remove the tumor, with or without radiation therapy.
- Drug therapy to stop the tumor from making hormones.
Pituitary Carcinomas
Treatment of pituitary carcinomas is palliative, to relieve symptoms and improve the quality of life. Treatment may include the following:
- Surgery (transsphenoidal surgery or craniotomy) to remove the cancer, with or without radiation therapy.
- Drug therapy to stop the tumor from making hormones.
- Chemotherapy.
Recurrent Pituitary Tumors
Treatment may include the following:
- Radiation therapy.
- A clinical trial of stereotactic radiation surgery.
Check the list of NCI-supported cancer clinical trials that are now accepting patients with pituitary tumor. For more specific results, refine the search by using other search features, such as the location of the trial, the type of treatment, or the name of the drug. Talk with your doctor about clinical trials that may be right for you. General information about clinical trials is available from the NCI website.
To Learn More About Pituitary Tumors
For more information from the National Cancer Institute about pituitary tumors, see the Pituitary Tumors Home Page.
For general cancer information and other resources from the National Cancer Institute, see the following:
- About Cancer
- Staging
- Chemotherapy and You: Support for People With Cancer
- Radiation Therapy and You: Support for People With Cancer
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors and Caregivers
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of pituitary tumors. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Date Last Modified") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials are listed in PDQ and can be found online at NCI's website. Many cancer doctors who take part in clinical trials are also listed in PDQ. For more information, call the Cancer Information Service 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Pituitary Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/pituitary/patient/pituitary-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389369]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 2,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2016-05-27
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.