Late Effects of Treatment for Childhood Cancer (PDQ®): Treatment - Health Professional Information [NCI]
Late Effects of Treatment for Childhood Cancer (PDQ®): Treatment - Health Professional Information [NCI]Skip to the navigationGeneral Information About Late Effects of Treatment for Childhood CancerDuring the past five decades, dramatic progress has been made in the development of curative therapy for pediatric malignancies. Long-term survival into adulthood is the expectation for more than 80% of children with access to contemporary therapies for pediatric malignancies.[1,2] The therapy responsible for this survival can also produce adverse long-term health-related outcomes, referred to as late effects, which manifest months to years after completion of cancer treatment. A variety of approaches have been used to advance knowledge about the very long-term morbidity associated with childhood cancer and its contribution to early mortality. These initiatives have utilized a spectrum of resources including investigation of data from the following: - Population-based registries.[3,4,5]
- Self-reported outcomes (provided through large-scale cohort studies).[6,7]
- Medical assessments.[8,9]
Studies reporting outcomes in survivors who have been well characterized in regards to clinical status and treatment exposures, and comprehensively ascertained for specific effects through medical assessments, typically provide the highest quality of data to establish the occurrence and risk profiles for late cancer treatment-related toxicity. Regardless of study methodology, it is important to consider selection and participation bias of the cohort studies in the context of the findings reported. Prevalence of Late Effects in Childhood Cancer Survivors Late effects are commonly experienced by adults who have survived childhood cancer; the prevalence of late effects increases as time from cancer diagnosis elapses. Population-based studies support excess hospital-related morbidity among childhood and young adult cancer survivors compared with age- and gender-matched controls.[3,4,5,10,11,12] Research has demonstrated that among adults treated for cancer during childhood, late effects contribute to a high burden of morbidity, including the following:[6,8,9,13,14] - 60% to more than 90% develop one or more chronic health conditions.
- 20% to 80% experience severe or life-threatening complications during adulthood.
The variability in prevalence is related to differences in the following: - Age and follow-up time of the cohorts studied.
- Methods and consistency of assessment (e.g., self-reported vs. risk-based medical evaluations).
Childhood Cancer Survivor Study (CCSS) investigators demonstrated that the elevated risk of morbidity and mortality among aging survivors in the cohort increases beyond the fourth decade of life. By age 50 years, the cumulative incidence of a self-reported severe, disabling, life-threatening, or fatal health condition was 53.6% among survivors, compared with 19.8% among a sibling control group. Among survivors who reached age 35 years without a previous severe, disabling, life-threatening, or fatal health condition, 25.9% experienced a new grade 3 to grade 5 health condition within 10 years, compared with 6.0% of healthy siblings.[6] The presence of serious, disabling, and life-threatening chronic health conditions adversely affects the health status of aging survivors, with the greatest impact on functional impairment and activity limitations. Female survivors demonstrate a steeper trajectory of age-dependent decline in health status compared with male survivors.[15] The even higher prevalence of late effects among clinically ascertained cohorts is related to the subclinical and undiagnosed conditions detected by screening and surveillance measures.[9]
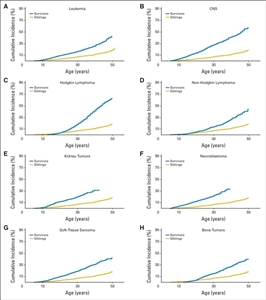
Figure 1. Cumulative incidence of chronic health conditions for severe, disabling, life-threatening, or fatal health conditions by primary childhood cancer diagnosis. (A) leukemia, (B) CNS tumors, (C) Hodgkin lymphoma, (D) non-Hodgkin lymphoma, (E) kidney tumors, (F) neuroblastoma, (G) soft tissue sarcoma, and (H) bone tumors. Gregory T. Armstrong, Toana Kawashima, Wendy Leisenring, Kayla Stratton, Marilyn Stovall, Melissa M. Hudson, Charles A. Sklar, Leslie L Robison, Kevin C. Oeffinger, Aging and Risk of Severe, Disabling, Life-Threatening, and Fatal Events in the Childhood Cancer Survivor Study, Journal of Clinical Oncology, volume 32, issue 12, pages 1218-1227. Reprinted with permission. © (2014) American Society of Clinical Oncology. All rights reserved.
CCSS investigators also evaluated the impact of race and ethnicity on late outcomes by comparing late mortality, subsequent neoplasms, and chronic health conditions in Hispanic (n = 750) and non-Hispanic black (n = 694) participants with non-Hispanic white participants (n = 12,397).[16] Cancer treatment did not account for disparities in mortality, chronic health conditions, or subsequent neoplasms observed among the groups. However, differences in socioeconomic status and cardiovascular risk factors affected risk. All-cause mortality was higher among non-Hispanic black participants than among other groups, but this difference disappeared after adjustment for socioeconomic status. Risks for diabetes were elevated among racial/ethnic minority groups even after adjustment for socioeconomic status and obesity. Non-Hispanic blacks had a higher likelihood of reporting cardiac conditions, but this risk diminished after adjusting for cardiovascular risk factors. Nonmelanoma skin cancer was not reported by non-Hispanic blacks, and Hispanic participants had a lower risk than did non-Hispanic white participants. Recognition of late effects, concurrent with advances in cancer biology, radiological sciences, and supportive care, has resulted in a change in the prevalence and spectrum of treatment effects. In an effort to reduce and prevent late effects, contemporary therapy for most pediatric malignancies has evolved to a risk-adapted approach that is assigned based on a variety of clinical, biological, and sometimes genetic factors. With the exception of survivors requiring intensive multimodality therapy for aggressive or refractory/relapsed malignancies, life-threatening treatment effects are relatively uncommon after contemporary therapy in early follow-up (up to 10 years after diagnosis). However, survivors still frequently experience life-altering morbidity related to effects of cancer treatment on endocrine, reproductive, musculoskeletal, and neurologic function. Mortality Late effects also contribute to an excess risk of premature death among long-term survivors of childhood cancer. Several studies of very large cohorts of survivors have reported early mortality among individuals treated for childhood cancer compared with age- and gender-matched general population controls. Relapsed/refractory primary cancer remains the most frequent cause of death, followed by excess cause-specific mortality from subsequent primary cancers and cardiac and pulmonary toxicity.[17,18,19,20,21,22]; [23][Level of evidence: 3iA] An analysis of the CCSS and Surveillance, Epidemiology, and End Results (SEER) study evaluating conditional survival demonstrated a subsequent 5-year survival rate of 92% or higher among most diagnoses at 5 years, 10 years, 15 years, and 20 years. Among those who had survived at least 5 years from diagnosis, the probability of all-cause mortality in the next 10 years was 8.8% in the CCSS and 10.6% in the SEER study, with neoplasms accounting for cause of death in approximately 75% of survivors.[24] Despite high premature morbidity rates, overall mortality has decreased over time.[17,25,26] This reduction is related to a decrease in deaths from the primary cancer without an associated increase in mortality from subsequent cancers or treatment-related toxicities. The former reflects improvements in therapeutic efficacy, and the latter reflects changes in therapy made subsequent to studying the causes of late effects. The expectation that mortality rates in survivors will continue to exceed those in the general population is based on the long-term sequelae that are likely to increase with attained age. If patients treated on therapeutic protocols are followed up for long periods into adulthood, it will be possible to evaluate the excess lifetime mortality in relation to specific therapeutic interventions. Monitoring for Late Effects Recognition of both acute and late modality-specific toxicity has motivated investigations evaluating the pathophysiology and prognostic factors for cancer treatment-related effects. The results of these studies have played an important role in the following areas:[17,25] - Changing pediatric cancer therapeutic approaches to reduce treatment-related mortality among survivors treated in more recent eras.
- The development of risk counseling and health screening recommendations for long-term survivors by identifying the clinical and treatment characteristics of those at highest risk of treatment complications.
The common late effects of pediatric cancer encompass several broad domains including: - Growth and development.
- Organ function.
- Reproductive capacity and health of offspring.
- Secondary carcinogenesis.
- Psychosocial sequelae related to the primary cancer, its treatment, or maladjustment associated with the cancer experience.
Late sequelae of therapy for childhood cancer can be anticipated based on therapeutic exposures, but the magnitude of risk and the manifestations in an individual patient are influenced by numerous factors. Factors that should be considered in the risk assessment for a given late effect include the following: Tumor-related factors
- Tumor location.
- Direct tissue effects.
- Tumor-induced organ dysfunction.
- Mechanical effects.
Treatment-related factors
- Radiation therapy: Total dose, fraction size, organ or tissue volume, type of machine energy.
- Chemotherapy: Agent type, dose-intensity, cumulative dose, schedule.
- Surgery: Technique, site.
- Hematopoietic cell transplantation.
- Use of combined modality therapy.
- Blood product transfusion.
- Management of chronic graft-versus-host disease.
Host-related factors
- Gender.
- Genetic predisposition.
- Premorbid health state.
- Developmental status.
- Age at diagnosis.
- Time from diagnosis/therapy.
- Inherent tissue sensitivities and capacity for normal tissue repair.
- Hormonal milieu.
- Function of organs not affected by cancer treatment.
- Socioeconomic status.
- Health habits.
Resources to Support Survivor Care Risk-based screening The need for long-term follow-up for childhood cancer survivors is supported by the American Society of Pediatric Hematology/Oncology, the International Society of Pediatric Oncology, the American Academy of Pediatrics, the Children's Oncology Group (COG), and the Institute of Medicine. A risk-based medical follow-up is recommended, which includes a systematic plan for lifelong screening, surveillance, and prevention that incorporates risk estimates based on the following:[27] - Previous cancer.
- Cancer therapy.
- Genetic predisposition.
- Lifestyle behaviors.
- Comorbid conditions.
Part of long-term follow-up is also focused on appropriate screening of educational and vocational progress. Specific treatments for childhood cancer, especially those that directly impact nervous system structures, may result in sensory, motor, and neurocognitive deficits that may have adverse consequences on functional status, educational attainment, and future vocational opportunities.[28] In support of this, a CCSS investigation observed the following:[29] - Treatment with cranial radiation doses of 25 Gy or higher was associated with higher odds of unemployment (health related: odds ratio [OR], 3.47; 95% confidence interval [CI], 2.54-4.74; seeking work: OR, 1.77; 95% CI, 1.15-2.71).
- Unemployed survivors reported higher levels of poor physical functioning than employed survivors, had lower education and income, and were more likely to be publicly insured than unemployed siblings.
These data emphasize the importance of facilitating survivor access to remedial services, which has been demonstrated to have a positive impact on education achievement,[30] which may in turn enhance vocational opportunities. In addition to risk-based screening for medical late effects, the impact of health behaviors on cancer-related health risks is also emphasized. Health-promoting behaviors are stressed for survivors of childhood cancer. Targeted educational efforts appear to be worthwhile in the following areas:[31] - Smoking, excess alcohol use, and illicit drug use to reduce the risk of organ toxicity and, potentially, subsequent neoplasms.
- Healthy dietary practices and active lifestyle to reduce treatment-related metabolic and cardiovascular complications.
Proactively addressing unhealthy and risky behaviors is pertinent, as several research investigations confirm that long-term survivors use tobacco and alcohol and have inactive lifestyles at higher rates than is ideal given their increased risk of cardiac, pulmonary, and metabolic late effects.[31,32,33] Access to risk-based survivor care Most childhood cancer survivors do not receive recommended risk-based care. The CCSS observed the following: - 88.8% of survivors reported receiving some form of medical care.[34]
- 31.5% reported receiving care that focused on their previous cancer (survivor-focused care).[34]
- 17.8% reported receiving survivor-focused care that included advice about risk reduction and discussion or ordering of screening tests.[34]
- Surveillance for new cases of cancer was very low in survivors at the highest risk of colon, breast, or skin cancer, suggesting that survivors and their physicians need education about the risk of subsequent neoplasms and recommended surveillance.[35]
- Sociodemographic factors have been linked to declining rates of follow-up care over time from diagnosis. CCSS participants who were male, had a household income of less than $20,000 per year, and had lower educational attainment (high school education or less) were more likely to report no care at their most recent follow-up survey. This trend is of concern because the prevalence of chronic health conditions increases with longer elapsed time from cancer diagnosis in adults treated for cancer during childhood.[36]
Access to health insurance appears to play an important role in risk-based survivor care.[37,38] Lack of access to health insurance affects the following: - Cancer-related visits. In a CCSS study, uninsured survivors were less likely than those privately insured to report a cancer-related visit (adjusted relative risk [RR], 0.83; 95% CI, 0.75-0.91) or a cancer center visit (adjusted RR, 0.83; 95% CI, 0.71-0.98). Uninsured survivors had lower levels of utilization in all measures of care than privately insured survivors. In contrast, publicly insured survivors were more likely to report a cancer-related visit (adjusted RR, 1.22; 95% CI, 1.11-1.35) or a cancer center visit (adjusted RR, 1.41; 95% CI, 1.18-1.70) than were privately insured survivors.[37]
- Health outcomes. In a study comparing health care outcomes for long-term survivors of adolescent and young adult (AYA) cancer with young adults who have a cancer history, the proportion of uninsured survivors did not differ between the two groups.[39]
- Financial burden. Subgroups of AYA survivors may be at additional risk of facing health care barriers. Younger survivors (aged 20-29 years), females, nonwhites, and survivors reporting poorer health faced more cost barriers, which may inhibit the early detection of late effects.[39]
Overall, lack of health insurance remains a significant concern for survivors of childhood cancer because of health issues, unemployment, and other societal factors.[40,41] Legislation, like the Health Insurance Portability and Accountability Act legislation,[42,43] has improved access and retention of health insurance among survivors, although the quality and limitations associated with these policies have not been well studied. Transition of Survivor Care Long-term follow-up programs Transition of care from the pediatric to adult health care setting is necessary for most childhood cancer survivors in the United States. When available, multidisciplinary long-term follow-up programs in the pediatric cancer center work collaboratively with community physicians to provide care for childhood cancer survivors. This type of shared-care has been proposed as the optimal model to facilitate coordination between the cancer center oncology team and community physician groups providing survivor care.[44] An essential service of long-term follow-up programs is the organization of an individualized survivorship care plan that includes the following: - Details about therapeutic interventions undertaken for childhood cancer and their potential health risks (e.g., chemotherapy type and cumulative dose, radiation treatment fields and dose, surgical procedures, blood product transfusions, and hematopoietic cell transplantation).
- Personalized health screening recommendations.
- Information about lifestyle factors that modify risks.
For survivors who have not been provided with this information, the COG offers a template that can be used by survivors to organize a personal treatment summary (refer to the COG Survivorship Guidelines, Appendix 1). COG Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers To facilitate survivor and provider access to succinct information to guide risk-based care, COG investigators have organized a compendium of exposure- and risk-based health surveillance recommendations, with the goal of standardizing the care of childhood cancer survivors.[45] The compendium of resources includes the following: - Long-Term Follow-Up Guidelines. COG Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers are appropriate for asymptomatic survivors presenting for routine exposure-based medical evaluation 2 or more years after completion of therapy.
- Health Links. Patient education materials called ‘‘Health Links'' provide detailed information on guideline-specific topics to enhance health maintenance and promotion among this population of cancer survivors.[46]
- Comprehensive reviews. Multidisciplinary system-based (e.g., cardiovascular, neurocognitive, and reproductive) task forces who are responsible for monitoring the literature, evaluating guideline content, and providing recommendations for guideline revisions as new information becomes available have published several comprehensive reviews that address specific late effects of childhood cancer.[47,48,49,50,51,52,53,54,55,56,57,58,59]
Information concerning late effects is summarized in tables throughout this summary. Several groups have undertaken research to evaluate the yield from risk-based screening as recommended by the COG and other pediatric oncology cooperative groups.[9,60,61] Pertinent considerations in interpreting the results of these studies include: - Variability in the cohort's age at treatment.
- Age at screening.
- Time from cancer treatment.
- Participation bias.
Collectively, these studies demonstrate that screening identifies a substantial proportion of individuals with previously unrecognized, treatment-related health complications of varying degrees of severity. Study results have also identified low-yield evaluations that have encouraged revisions of screening recommendations. Ongoing research is evaluating cost effectiveness of screening in the context of consideration of benefits, risks, and harms. References:
-
Jemal A, Siegel R, Xu J, et al.: Cancer statistics, 2010. CA Cancer J Clin 60 (5): 277-300, 2010 Sep-Oct.
-
Howlader N, Noone AM, Krapcho M, et al., eds.: SEER Cancer Statistics Review, 1975-2010. Bethesda, Md: National Cancer Institute, 2013. Also available online. Last accessed January 27, 2017.
-
Lorenzi MF, Xie L, Rogers PC, et al.: Hospital-related morbidity among childhood cancer survivors in British Columbia, Canada: report of the childhood, adolescent, young adult cancer survivors (CAYACS) program. Int J Cancer 128 (7): 1624-31, 2011.
-
Mols F, Helfenrath KA, Vingerhoets AJ, et al.: Increased health care utilization among long-term cancer survivors compared to the average Dutch population: a population-based study. Int J Cancer 121 (4): 871-7, 2007.
-
Rebholz CE, Reulen RC, Toogood AA, et al.: Health care use of long-term survivors of childhood cancer: the British Childhood Cancer Survivor Study. J Clin Oncol 29 (31): 4181-8, 2011.
-
Armstrong GT, Kawashima T, Leisenring W, et al.: Aging and risk of severe, disabling, life-threatening, and fatal events in the childhood cancer survivor study. J Clin Oncol 32 (12): 1218-27, 2014.
-
Oeffinger KC, Mertens AC, Sklar CA, et al.: Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355 (15): 1572-82, 2006.
-
Geenen MM, Cardous-Ubbink MC, Kremer LC, et al.: Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA 297 (24): 2705-15, 2007.
-
Hudson MM, Ness KK, Gurney JG, et al.: Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309 (22): 2371-81, 2013.
-
Sun CL, Francisco L, Kawashima T, et al.: Prevalence and predictors of chronic health conditions after hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study. Blood 116 (17): 3129-39; quiz 3377, 2010.
-
Kurt BA, Nolan VG, Ness KK, et al.: Hospitalization rates among survivors of childhood cancer in the Childhood Cancer Survivor Study cohort. Pediatr Blood Cancer 59 (1): 126-32, 2012.
-
Zhang Y, Lorenzi MF, Goddard K, et al.: Late morbidity leading to hospitalization among 5-year survivors of young adult cancer: a report of the childhood, adolescent and young adult cancer survivors research program. Int J Cancer 134 (5): 1174-82, 2014.
-
Berbis J, Michel G, Chastagner P, et al.: A French cohort of childhood leukemia survivors: impact of hematopoietic stem cell transplantation on health status and quality of life. Biol Blood Marrow Transplant 19 (7): 1065-72, 2013.
-
Phillips SM, Padgett LS, Leisenring WM, et al.: Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiol Biomarkers Prev 24 (4): 653-63, 2015.
-
Hudson MM, Oeffinger KC, Jones K, et al.: Age-dependent changes in health status in the Childhood Cancer Survivor cohort. J Clin Oncol 33 (5): 479-91, 2015.
-
Liu Q, Leisenring WM, Ness KK, et al.: Racial/Ethnic Differences in Adverse Outcomes Among Childhood Cancer Survivors: The Childhood Cancer Survivor Study. J Clin Oncol 34 (14): 1634-43, 2016.
-
Armstrong GT, Pan Z, Ness KK, et al.: Temporal trends in cause-specific late mortality among 5-year survivors of childhood cancer. J Clin Oncol 28 (7): 1224-31, 2010.
-
Bhatia S, Robison LL, Francisco L, et al.: Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the Bone Marrow Transplant Survivor Study. Blood 105 (11): 4215-22, 2005.
-
MacArthur AC, Spinelli JJ, Rogers PC, et al.: Mortality among 5-year survivors of cancer diagnosed during childhood or adolescence in British Columbia, Canada. Pediatr Blood Cancer 48 (4): 460-7, 2007.
-
Tukenova M, Guibout C, Hawkins M, et al.: Radiation therapy and late mortality from second sarcoma, carcinoma, and hematological malignancies after a solid cancer in childhood. Int J Radiat Oncol Biol Phys 80 (2): 339-46, 2011.
-
Prasad PK, Signorello LB, Friedman DL, et al.: Long-term non-cancer mortality in pediatric and young adult cancer survivors in Finland. Pediatr Blood Cancer 58 (3): 421-7, 2012.
-
Youn P, Milano MT, Constine LS, et al.: Long-term cause-specific mortality in survivors of adolescent and young adult bone and soft tissue sarcoma: a population-based study of 28,844 patients. Cancer 120 (15): 2334-42, 2014.
-
Reulen RC, Winter DL, Frobisher C, et al.: Long-term cause-specific mortality among survivors of childhood cancer. JAMA 304 (2): 172-9, 2010.
-
Mertens AC, Yong J, Dietz AC, et al.: Conditional survival in pediatric malignancies: analysis of data from the Childhood Cancer Survivor Study and the Surveillance, Epidemiology, and End Results Program. Cancer 121 (7): 1108-17, 2015.
-
Yeh JM, Nekhlyudov L, Goldie SJ, et al.: A model-based estimate of cumulative excess mortality in survivors of childhood cancer. Ann Intern Med 152 (7): 409-17, W131-8, 2010.
-
Armstrong GT, Chen Y, Yasui Y, et al.: Reduction in Late Mortality among 5-Year Survivors of Childhood Cancer. N Engl J Med 374 (9): 833-42, 2016.
-
McCabe MS, Partridge AH, Grunfeld E, et al.: Risk-based health care, the cancer survivor, the oncologist, and the primary care physician. Semin Oncol 40 (6): 804-12, 2013.
-
Hudson MM, Mulrooney DA, Bowers DC, et al.: High-risk populations identified in Childhood Cancer Survivor Study investigations: implications for risk-based surveillance. J Clin Oncol 27 (14): 2405-14, 2009.
-
Kirchhoff AC, Leisenring W, Krull KR, et al.: Unemployment among adult survivors of childhood cancer: a report from the childhood cancer survivor study. Med Care 48 (11): 1015-25, 2010.
-
Mitby PA, Robison LL, Whitton JA, et al.: Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer 97 (4): 1115-26, 2003.
-
Nathan PC, Ford JS, Henderson TO, et al.: Health behaviors, medical care, and interventions to promote healthy living in the Childhood Cancer Survivor Study cohort. J Clin Oncol 27 (14): 2363-73, 2009.
-
Schultz KA, Chen L, Chen Z, et al.: Health and risk behaviors in survivors of childhood acute myeloid leukemia: a report from the Children's Oncology Group. Pediatr Blood Cancer 55 (1): 157-64, 2010.
-
Tercyak KP, Donze JR, Prahlad S, et al.: Multiple behavioral risk factors among adolescent survivors of childhood cancer in the Survivor Health and Resilience Education (SHARE) program. Pediatr Blood Cancer 47 (6): 825-30, 2006.
-
Nathan PC, Greenberg ML, Ness KK, et al.: Medical care in long-term survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 26 (27): 4401-9, 2008.
-
Nathan PC, Ness KK, Mahoney MC, et al.: Screening and surveillance for second malignant neoplasms in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Ann Intern Med 153 (7): 442-51, 2010.
-
Casillas J, Oeffinger KC, Hudson MM, et al.: Identifying Predictors of Longitudinal Decline in the Level of Medical Care Received by Adult Survivors of Childhood Cancer: A Report from the Childhood Cancer Survivor Study. Health Serv Res 50 (4): 1021-42, 2015.
-
Casillas J, Castellino SM, Hudson MM, et al.: Impact of insurance type on survivor-focused and general preventive health care utilization in adult survivors of childhood cancer: the Childhood Cancer Survivor Study (CCSS). Cancer 117 (9): 1966-75, 2011.
-
Keegan TH, Tao L, DeRouen MC, et al.: Medical care in adolescents and young adult cancer survivors: what are the biggest access-related barriers? J Cancer Surviv 8 (2): 282-92, 2014.
-
Kirchhoff AC, Lyles CR, Fluchel M, et al.: Limitations in health care access and utilization among long-term survivors of adolescent and young adult cancer. Cancer 118 (23): 5964-72, 2012.
-
Crom DB, Lensing SY, Rai SN, et al.: Marriage, employment, and health insurance in adult survivors of childhood cancer. J Cancer Surviv 1 (3): 237-45, 2007.
-
Pui CH, Cheng C, Leung W, et al.: Extended follow-up of long-term survivors of childhood acute lymphoblastic leukemia. N Engl J Med 349 (7): 640-9, 2003.
-
Park ER, Kirchhoff AC, Zallen JP, et al.: Childhood Cancer Survivor Study participants' perceptions and knowledge of health insurance coverage: implications for the Affordable Care Act. J Cancer Surviv 6 (3): 251-9, 2012.
-
Warner EL, Park ER, Stroup A, et al.: Childhood cancer survivors' familiarity with and opinions of the Patient Protection and Affordable Care Act. J Oncol Pract 9 (5): 246-50, 2013.
-
Oeffinger KC, McCabe MS: Models for delivering survivorship care. J Clin Oncol 24 (32): 5117-24, 2006.
-
Landier W, Bhatia S, Eshelman DA, et al.: Development of risk-based guidelines for pediatric cancer survivors: the Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol 22 (24): 4979-90, 2004.
-
Eshelman D, Landier W, Sweeney T, et al.: Facilitating care for childhood cancer survivors: integrating children's oncology group long-term follow-up guidelines and health links in clinical practice. J Pediatr Oncol Nurs 21 (5): 271-80, 2004 Sep-Oct.
-
Castellino S, Muir A, Shah A, et al.: Hepato-biliary late effects in survivors of childhood and adolescent cancer: a report from the Children's Oncology Group. Pediatr Blood Cancer 54 (5): 663-9, 2010.
-
Henderson TO, Amsterdam A, Bhatia S, et al.: Systematic review: surveillance for breast cancer in women treated with chest radiation for childhood, adolescent, or young adult cancer. Ann Intern Med 152 (7): 444-55; W144-54, 2010.
-
Jones DP, Spunt SL, Green D, et al.: Renal late effects in patients treated for cancer in childhood: a report from the Children's Oncology Group. Pediatr Blood Cancer 51 (6): 724-31, 2008.
-
Liles A, Blatt J, Morris D, et al.: Monitoring pulmonary complications in long-term childhood cancer survivors: guidelines for the primary care physician. Cleve Clin J Med 75 (7): 531-9, 2008.
-
Nandagopal R, Laverdière C, Mulrooney D, et al.: Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res 69 (2): 65-74, 2008.
-
Nathan PC, Patel SK, Dilley K, et al.: Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children's Oncology Group. Arch Pediatr Adolesc Med 161 (8): 798-806, 2007.
-
Ritchey M, Ferrer F, Shearer P, et al.: Late effects on the urinary bladder in patients treated for cancer in childhood: a report from the Children's Oncology Group. Pediatr Blood Cancer 52 (4): 439-46, 2009.
-
Shankar SM, Marina N, Hudson MM, et al.: Monitoring for cardiovascular disease in survivors of childhood cancer: report from the Cardiovascular Disease Task Force of the Children's Oncology Group. Pediatrics 121 (2): e387-96, 2008.
-
Wasilewski-Masker K, Kaste SC, Hudson MM, et al.: Bone mineral density deficits in survivors of childhood cancer: long-term follow-up guidelines and review of the literature. Pediatrics 121 (3): e705-13, 2008.
-
Metzger ML, Meacham LR, Patterson B, et al.: Female reproductive health after childhood, adolescent, and young adult cancers: guidelines for the assessment and management of female reproductive complications. J Clin Oncol 31 (9): 1239-47, 2013.
-
Kenney LB, Cohen LE, Shnorhavorian M, et al.: Male reproductive health after childhood, adolescent, and young adult cancers: a report from the Children's Oncology Group. J Clin Oncol 30 (27): 3408-16, 2012.
-
Effinger KE, Migliorati CA, Hudson MM, et al.: Oral and dental late effects in survivors of childhood cancer: a Children's Oncology Group report. Support Care Cancer 22 (7): 2009-19, 2014.
-
Bass JK, Knight KR, Yock TI, et al.: Evaluation and Management of Hearing Loss in Survivors of Childhood and Adolescent Cancers: A Report From the Children's Oncology Group. Pediatr Blood Cancer 63 (7): 1152-62, 2016.
-
Landier W, Armenian SH, Lee J, et al.: Yield of screening for long-term complications using the children's oncology group long-term follow-up guidelines. J Clin Oncol 30 (35): 4401-8, 2012.
-
Wasilewski-Masker K, Mertens AC, Patterson B, et al.: Severity of health conditions identified in a pediatric cancer survivor program. Pediatr Blood Cancer 54 (7): 976-82, 2010.
Subsequent NeoplasmsSubsequent neoplasms (SNs), which may be benign or malignant, are defined as histologically distinct neoplasms developing at least 2 months after completion of treatment for the primary malignancy. Childhood cancer survivors have an increased risk of developing SNs that varies according to the following: - Host factors (e.g., genetics, immune function, hormone status).
- Primary cancer therapy.
- Environmental exposures.
- Lifestyle factors.
SNs are the leading cause of nonrelapse late mortality (standardized mortality ratio, 15.2; 95% confidence interval [CI], 13.9-16.6).[1] The Childhood Cancer Survivor Study (CCSS) reported the following 30-year cumulative incidence rates:[2] - All SNs-20.5% (95% CI, 19.1%-21.8%).
- SNs with malignant histologies (excluding nonmelanoma skin cancer [NMSC])-7.9% (95% CI, 7.2%-8.5%).
- NMSC-9.1% (95% CI, 8.1%-10.1%).
- Meningioma-3.1% (95% CI, 2.5%-3.8%).
This represents a sixfold increased risk of SNs among cancer survivors, compared with the general population.[2] The excess risk of SNs persists even after the age of 40 years.[3] At the age of 55 years, the cumulative incidence of any new SN (including malignant neoplasms, NMSCs, benign meningiomas, and other benign neoplasms) occurring after the age of 40 years was 34.6% in the CCSS cohort. The incidence of malignant SNs was 16.3%. Female gender and therapeutic radiation exposure were associated with an increased risk of subsequent malignant neoplasms in multivariate analysis. Moreover, prolonged follow-up has established that multiple SNs are common among aging childhood cancer survivors.[4,5] The development of an SN is likely multifactorial in etiology and results from a combination of influences including gene-environment and gene-gene interactions. Outcome after the diagnosis of an SN is variable, as treatment for some histological subtypes may be compromised if childhood cancer therapy included cumulative doses of agents and modalities at the threshold of tissue tolerance.[6] The incidence and type of SNs depend on the following: - Primary cancer diagnosis.
- Type of therapy received.
- Presence of genetic conditions.
Unique associations with specific therapeutic exposures have resulted in the classification of SNs into the following two distinct groups: - Chemotherapy-related myelodysplastic syndrome and acute myeloid leukemia (t-MDS/AML).
- Radiation-related solid SNs.
Therapy-Related Myelodysplastic Syndrome and Leukemia Therapy-related myelodysplastic syndrome and acute myeloid leukemia (t-MDS/AML) has been reported after treatment of Hodgkin lymphoma (HL), acute lymphoblastic leukemia (ALL), and sarcomas, with the cumulative incidence approaching 2% at 15 years after therapy.[7,8,9,10] Characteristics of t-MDS/AML include the following:[7,11,12] - A short latency (<10 years from primary cancer diagnosis). The risk of t-MDS/AML plateaus after 10 to 15 years. Although the risk of subsequent leukemia remains significantly elevated beyond 15 years from primary diagnosis (standardized incidence ratio [SIR], 3.5; 95% CI, 1.9-6.0), these events are relatively rare, with an absolute excess risk of 0.02 cases per 1,000 person-years.[12]
- An association with alkylating agents and/or topoisomerase II inhibitors.
t-MDS/AML is a clonal disorder characterized by distinct chromosomal changes. The following two types of t-MDS/AML are recognized by the World Health Organization classification:[13] - Alkylating agent-related type: Alkylating agents associated with t-MDS/AML include cyclophosphamide, ifosfamide, mechlorethamine, melphalan, busulfan, nitrosoureas, chlorambucil, and dacarbazine.[14]
The risk of alkylating agent-related t-MDS/AML is dose dependent, with a latency of 3 to 5 years after exposure; it is associated with abnormalities involving chromosomes 5 (-5/del(5q)) and 7 (-7/del(7q)).[14] - Topoisomerase II inhibitor-related type: Topoisomerase II inhibitor agents include etoposide, teniposide, and anthracycline-related drugs.
Most of the translocations observed in patients exposed to topoisomerase II inhibitors disrupt a breakpoint cluster region between exons 5 and 11 of the band 11q23 and fuse mixed lineage leukemia with a partner gene.[14] Topoisomerase II inhibitor-related t-AML presents as overt leukemia after a latency of 6 months to 3 years and is associated with balanced translocations involving chromosome bands 11q23 or 21q22.[15]
Therapy-Related Solid Neoplasms Therapy-related solid SNs represent 80% of all SNs and demonstrate a strong relationship with radiation exposure and are characterized by a latency that exceeds 10 years. The risk of solid SNs continues to increase with longer follow-up. The risk of solid SNs is highest when the following occur:[2] - Radiation exposure at a younger age.
- High total dose of radiation.
- Longer period of follow-up after radiation exposure.
The histological subtypes of solid SNs encompass a neoplastic spectrum ranging from benign and low-grade malignant lesions (e.g., NMSC, meningiomas) to high-grade malignancies (e.g., breast cancers, glioblastomas).[2,9,16,17,18,19,20] Solid SNs in childhood cancer survivors most commonly involve the following: [2,7,9,17,21,22] - Breast.
- Thyroid.
- Central nervous system (CNS).
- Bone and soft tissue.
With more prolonged follow-up of adult survivors of childhood cancer cohorts, epithelial neoplasms have been observed in the following:[2,7,16] - Lung.
- Gastrointestinal tract.
Benign and low-grade SNs, including NMSCs and meningiomas, have also been observed with increasing prevalence in survivors who were treated with radiation therapy for childhood cancer.[2,17,18] In addition to radiation exposure, exposure to certain anticancer agents may result in solid SNs. In recipients of a hematopoietic cell transplant conditioned with high-dose busulfan and cyclophosphamide (Bu-Cy), the cumulative incidence of new solid cancers appears to be similar regardless of exposure to radiation. In a registry-based, retrospective, cohort study, Bu-Cy conditioning without total-body irradiation (TBI) was associated with higher risks of solid SNs than in the general population. Chronic graft-versus-host disease increased the risk of SNs, especially those involving the oral cavity.[23] Some well-established solid SNs include the following:[24] - Breast cancer: Breast cancer is the most common therapy-related solid SN after HL, largely due to the high-dose of chest radiation used to treat HL (SIR of subsequent breast cancer, 25-55).[7,25] The following has been observed in female survivors of childhood HL:
- Excess risk has been reported in female HL survivors treated with high-dose, extended-volume radiation at age 30 years or younger.[26] Emerging data indicate that females treated with low-dose, involved-field radiation also exhibit excess breast cancer risk.[27]
- For female HL patients treated with radiation therapy to the chest before age 16 years, the cumulative incidence of breast cancer approaches 20% by age 45 years.[7]
- The latency period after chest irradiation ranges from 8 to 10 years, and the risk of subsequent breast cancer increases in a linear fashion with radiation dose (P for trend < .001).[28]
Radiation-induced breast cancer has been reported in one population-based study to have more adverse clinicopathological features, as evidenced by a twofold increased risk of estrogen receptor-negative, progesterone receptor-negative breast cancer observed among 15-year HL survivors, compared with women who had sporadic breast cancer.[29] In a Stanford investigation evaluating the histological subtypes of breast cancer among 65 patients treated with radiation therapy for HL (median age, 23 years at HL diagnosis), breast cancers arising in previously irradiated breast tissue were more likely to be triple negative than were age-matched sporadic invasive cancers, and less likely to be hormone receptor-positive breast cancer, particularly hormone receptor-positive/human epidermal growth factor receptor 2-positive breast cancer.[30] These findings are in contrast to other smaller hospital-based, case-control studies of breast cancer among HL survivors that have not identified a significant variation in hormone receptor status when compared with primary breast cancer controls. Previous studies have also not demonstrated significant difference in overall risk of high-grade versus low-grade tumors.[31,32,33] Treatment with higher cumulative doses of alkylating agents and ovarian radiation greater than or equal to 5 Gy (exposures predisposing to premature menopause) have been correlated with reductions in breast cancer risk, underscoring the potential contribution of hormonal stimulation on breast carcinogenesis.[34,35] Most data describing the risk of radiation-associated breast cancer are based on patients treated for HL, with doses ranging from 15 Gy to 50 Gy. Lower radiation doses used to treat cancer metastatic to the lungs (e.g., Wilms tumor, sarcoma) that expose the breast tissues also appear to increase the risk of breast cancer. In 116 children in the CCSS cohort treated with 2 Gy to 20 Gy to the lungs (median, 14 Gy), the SIR for breast cancer was 43.6 (95% CI, 27.1-70.1).[36] In a report of 2,492 female participants in the National Wilms Tumor Studies 1 through 4 (1969-1995), 16 of 369 women who received chest irradiation for metastatic Wilms tumor developed invasive breast cancer (cumulative risk at age 40 years, 14.8% [95% CI, 1.3-7.41]). The SIR of 27.6 (95% CI, 16.1-44.2) was based on 5,010 person-years of follow-up. Of the 369 patients, radiation doses to the chest were lower than 12 Gy in 4%, 12 Gy in 64%, 13 Gy to 15 Gy in 19%, and higher than 15 Gy in 13% of patients. For all patients who developed breast cancer (with or without chest irradiation), the median age at first breast cancer diagnosis was 34.3 years (range, 15.5-48.4) and the median time from Wilms tumor diagnosis was 27.1 years (range, 7.9-35.7).[37] Although currently available evidence is insufficient to demonstrate a survival benefit from the initiation of breast cancer surveillance in women treated with radiation therapy to the chest for childhood cancer, interventions to promote detection of small and early-stage tumors may improve prognosis, particularly for those who may have more limited treatment options because of previous exposure to radiation or anthracyclines. - Childhood sarcoma or leukemia survivors not exposed to chest radiation also have an increased risk of breast cancer at a young age. CCSS investigators observed a fourfold excess risk (SIR, 4.0; 95% CI, 3.0-5.3) of breast cancer compared with rates in the general population among 3,768 female participants who did not receive chest radiation. Breast cancer risk was highest among sarcoma (SIR, 5.3; 95% CI, 3.6-7.8) and leukemia (SIR, 4.1; 95% CI, 2.4-6.9) survivors, for whom the cumulative incidence of breast cancer was estimated to be 5.8% and 6.3%, respectively, by age 45 years. Treatment with alkylating agents and anthracyclines increased the risk of breast cancer in a dose-dependent manner.[38]
- Thyroid cancer: Thyroid cancer is observed after the following:[2,7,39]
- Neck radiation therapy for HL, ALL, and brain tumors.
- Iodine I 131 metaiodobenzylguanidine (131 I-mIBG) treatment for neuroblastoma.
- TBI for hematopoietic stem cell transplantation.
The risk of thyroid cancer has been reported to be 18-fold that of the general population.[40] Significant modifiers of the radiation-related risk of thyroid cancer include the following:[41,42] - Female gender.
- Younger age at exposure.
- Longer time since exposure.
- Radiation dose. A linear dose-response relationship between radiation exposure and thyroid cancer is observed up to 29 Gy, with a decline in the odds ratio (OR) at higher doses, especially in children younger than 10 years at treatment, demonstrating evidence for a cell kill effect.[41,43]
(Refer to the Thyroid nodules section of this summary for information on detecting thyroid nodules and thyroid cancer.) - CNS tumors: Brain tumors develop after cranial irradiation for histologically distinct brain tumors [17] or for management of disease among ALL or non-Hodgkin lymphoma patients.[8,44] SIRs reported for subsequent CNS neoplasms after treatment for childhood cancer range from 8.1 to 52.3 across studies.[45]
The risk of subsequent brain tumors demonstrates a linear relationship with radiation dose.[2,17] - The risk of meningioma after radiation not only increases with radiation dose but also with increased dose of intrathecal methotrexate.[46]
- Cavernomas have also been reported with considerable frequency after CNS irradiation but have been speculated to result from angiogenic processes as opposed to true tumorigenesis.[47,48,49]
Despite the well-established increased risk of subsequent CNS neoplasms among childhood cancer survivors treated with cranial irradiation, the current literature is insufficient to evaluate the potential harms and benefits of routine screening for these lesions.[45] - Bone and soft tissue tumors: The risk of subsequent bone tumors has been reported to be 133-fold that of the general population, with an estimated 20-year cumulative risk of 2.8%.[50] Survivors of hereditary retinoblastoma, Ewing sarcoma, and other malignant bone tumors are at a particularly increased risk.[51,52]
Radiation therapy is associated with a linear dose-response relationship.[51,53] After adjustment for radiation therapy, treatment with alkylating agents has also been linked to bone cancer, with the risk increasing with cumulative drug exposure.[51] These data from earlier studies concur with the following data observed by the CCSS and other investigators: - In a CCSS cohort, an increased risk of subsequent bone or soft tissue sarcoma was associated with radiation therapy, a primary diagnosis of sarcoma, a history of other SNs, and treatment with higher doses of anthracyclines or alkylating agents.[54] The 30-year cumulative incidence of subsequent sarcoma in CCSS participants was 1.08% for survivors who received radiation therapy and 0.5% for survivors who did not receive radiation therapy.[54]
- In a retrospective cohort of 4,171 survivors of a solid childhood cancer treated between 1942 and 1986 (median follow-up, 26 years), dose-risk modeling demonstrated that the risk of bone sarcoma increased slightly up to a cumulative organ-absorbed radiation dose of 15 Gy (hazard ratio [HR], 8.2; 95 % CI, 1.6-42.9) and then rapidly increased for higher radiation doses (HR for 30 Gy or more, 117.9; 95 % CI, 36.5-380.6), compared with patients not treated with radiation therapy. The excess relative risk per Gy in this model was 1.77 (95 % CI, 0.62-5.94).[53]
- In survivors of bilateral retinoblastoma, the most common SNs seen are sarcomas, specifically osteosarcoma.[55,56,57] The contribution of chemotherapy to solid malignancy carcinogenesis was highlighted in a long-term follow-up study of 906 5-year hereditary retinoblastoma survivors who were diagnosed between 1914 and 1996 and observed through 2009.[52] Treatment with alkylating agents significantly increased risk of subsequent bone tumors (HR, 1.60; 95% CI, 1.03-2.49) and leiomyosarcoma (HR, 2.67; 95% CI, 1.22-5.85) among members of the cohort. Leiomyosarcoma occurrence was more common after treatment with alkylating agent chemotherapy and radiation therapy compared with radiation therapy alone (5.8% vs. 1.6% at age 40 years; P = .01).
Soft tissue sarcomas can be of various histologic subtypes, including nonrhabdomyosarcoma soft tissue sarcomas, rhabdomyosarcoma, malignant peripheral nerve sheath tumors, Ewing/primitive neuroectodermal tumors, and other rare types. The CCSS reported the following on 105 cases and 422 matched controls in a nested case-control study of 14,372 childhood cancer survivors:[58] - Soft tissue sarcomas occurred at a median of 11.8 years (range, 5.3-31.3 years) from original diagnoses.
- Any exposure to radiation was associated with increased risk of soft tissue sarcoma (OR, 4.1; 95% CI, 1.8-9.5), which demonstrated a linear dose-response relationship.
- Anthracycline exposure was associated with soft tissue sarcoma risk (OR, 3.5; 95% CI, 1.6-7.7), independent of radiation dose.
- Skin cancer:
Nonmelanoma skin cancers (NMSCs) represent one of the most common SNs among childhood cancer survivors and exhibit a strong association with radiation therapy.[59] The CCSS has observed the following: The occurrence of an NMSC as the first SN has been reported to identify a population at high risk of a future invasive malignant SN.[4] CCSS investigators observed a cumulative incidence of a malignant neoplasm of 20.3% (95% CI, 13.0%-27.6%) at 15 years among radiation-exposed survivors who developed NMSC as a first SN compared with 10.7% (95% CI, 7.2%-14.2%) whose first SN was an invasive malignancy. Malignant melanoma has also been reported as an SN in childhood cancer survivor cohorts, although at a much lower incidence than NMSCs. A systematic review including data from 19 original studies (total N = 151,575 survivors; median follow-up of 13 years) observed an incidence of 10.8 cases of malignant melanoma per 100,000 childhood cancer survivors per year.[61] Risk factors for malignant melanoma identified among these studies include the following:[61] - Radiation therapy.
- Combination of alkylating agents and antimitotic drugs.
Melanomas most frequently developed in survivors of HL, hereditary retinoblastoma, soft tissue sarcoma, and gonadal tumors, but the relatively small number of survivors represented in the relevant studies preclude assessment of melanoma risk among other types of childhood cancer.[61] CCSS investigators observed an approximate 2.5-fold increased risk (SIR, 2.42; 95% CI, 1.77-3.23) of melanoma among members of their cohort (median time to development, 21.0 years). The cumulative incidence of first subsequent melanoma at 35 years from initial cancer diagnosis was 0.55% (95% CI, 0.37-0.73), and absolute excess risk was 0.10 per 1,000 person-years (95% CI, 0.05-0.15). Family history of cancer, demographic, or treatment-related factors did not predict risk of melanoma.[62] - Lung cancer: Among pediatric childhood cancer survivor cohorts, lung cancer represents a relatively uncommon SN; the 30-year cumulative incidence of lung cancer among CCSS participants was 0.1% (95% CI, 0.0%-0.2%).[2] The following has been observed in adult survivors of childhood HL:[63]
- Lung cancer has been reported after chest irradiation for HL. The risk increases in association with longer elapsed time from diagnosis.
- Smoking has been linked with the occurrence of lung cancer that develops after radiation therapy for HL. The increase in risk of lung cancer with increasing radiation dose is greater among patients who smoke after exposure to radiation than among those who refrain from smoking (P = .04).
- Gastrointestinal (GI) cancer: There is emerging evidence that childhood cancer survivors develop GI malignancies more frequently and at a younger age than the general population.[7,64,65,66]
The Late Effects Study Group reported a 63.9-fold increased risk of gastric cancers and 36.4-fold increased risk of colorectal cancers in adult survivors of childhood HL. In addition to previous radiation therapy, younger age (0-5 years) at the time of the primary cancer therapy significantly increased risk.[7] In a French and British cohort-nested, case-control study of childhood solid cancer survivors diagnosed before age 17 years, the risk of developing an SN in the digestive organs varied with therapy. The following was also observed:[64] - The risk of GI cancer was 9.7-fold higher than in population controls.
- The SNs most often involved the colon/rectum (42%), liver (24%), and stomach (19%).
- A strong radiation dose-response relationship, with an OR of 5.2 (95% CI, 1.7-16.0) for local radiation doses between 10 Gy and 29 Gy and 9.6 (95% CI, 2.6-35.2) for doses of 30 Gy and above, compared with the dose response in survivors who had not received radiation therapy.
- Chemotherapy alone and combined-modality therapy were associated with a significantly increased risk of developing a GI SN (SIR, 9.1; 95% CI, 2.3-23.6; SIR 29.0; 95% CI, 20.5-39.8).
CCSS investigators reported a 4.6-fold higher risk of GI SNs among their study participants than in the general population (95% CI, 3.4-6.1). They also reported the following:[65] - The SNs most often involved the colon (39%), rectum/anus (16%), liver (18%), and stomach (13%).
- The SIR for colorectal cancer was 4.2 (CI, 2.8-6.3).
- The most prevalent GI SN histology was adenocarcinoma (56%).
- The highest risk of GI SNs was associated with abdominal irradiation (SIR, 11.2; CI, 7.6-16.4), but survivors not exposed to radiation also had a significantly increased risk (SIR, 2.4; CI, 1.4-3.9).
- High-dose procarbazine (relative risk [RR], 3.2; CI 1.1-9.4) and platinum drugs (RR, 7.6; CI, 2.3-25.5) independently increased the risk of GI SNs.
St. Jude Children's Research Hospital investigators observed that the SIR for subsequent colorectal carcinoma was 10.9 (95% CI, 6.6-17.0) compared with U.S. population controls. Investigators also observed the following:[66] - Incidence of a subsequent colorectal carcinoma increased steeply with advancing age, with a 40-year cumulative incidence of 1.4% ± 0.53% among the entire cohort (N = 13,048) and 2.3% ± 0.83% for 5-year survivors.
- Colorectal carcinoma risk increased by 70% with each 10 Gy increase in radiation dose, and increasing radiation volume also increased risk.
- Treatment with alkylating agent chemotherapy was also associated with an 8.8-fold excess risk of subsequent colorectal carcinoma.
Collectively, these studies support the need for initiation of colorectal carcinoma surveillance at a young age among survivors receiving high-risk exposures.[7,64,65,66] - Renal carcinoma: Consistent with reports among survivors of adult-onset cancer, an increased risk of renal carcinoma has been observed in survivors of childhood cancer.[67,68,69] CCSS investigators reported a significant excess of subsequent renal carcinoma among 14,358 5-year survivors in the cohort (SIR, 8.0; 95% CI, 5.2-11.7) compared with the general population.[67] The reported overall absolute excess risk of 8.4 per 105 person-years indicates that these cases are relatively rare. Highest risk was observed among the following:
- Neuroblastoma survivors (SIR, 85.8; 95% CI, 38.4-175.2).[67] Radiation has been hypothesized to predispose children with high-risk neuroblastoma to renal carcinoma.[70]
- Those treated with renal-directed radiation therapy of 5 Gy or greater (RR, 3.8; 95% CI, 1.6-9.3).[67]
- Those treated with platinum-based chemotherapy (RR, 3.5; 95% CI, 1.0-11.2).[67] Cases of secondary renal carcinoma associated with Xp11.2 translocations and TFE3 gene fusions have also been reported and suggest that cytotoxic chemotherapy may contribute to renal carcinogenesis.[71,72]
Underlying genetic predisposition may also play a role because rare cases of renal carcinoma have been observed in children with tuberous sclerosis.[67]
Subsequent Neoplasms and Genetic Susceptibility Literature clearly supports the role of chemotherapy and radiation therapy in the development of SNs. However, interindividual variability exists, suggesting that genetic variation has a role in susceptibility to genotoxic exposures, or that genetic susceptibility syndrome confers an increased risk of cancer, such as Li-Fraumeni syndrome.[73] Previous studies have demonstrated that childhood cancer survivors with a family history of Li-Fraumeni syndrome in particular, or a family history of cancer, carry an increased risk of developing an SN.[74,75] The risk of SNs could potentially be modified by mutations in high-penetrance genes that lead to these serious genetic diseases (e.g., Li-Fraumeni syndrome).[75] However, the attributable risk is expected to be very small because of the extremely low prevalence of mutations in high-penetrance genes. Table 1 below summarizes the spectrum of neoplasms, affected genes, and Mendelian mode of inheritance of selected syndromes of inherited cancer predisposition. Table 1. Selected Syndromes of Inherited Cancer Predispositiona| Syndrome | Major Tumor Types | Affected Gene | Mode of Inheritance |
|---|
| AML = acute myeloid leukemia; MDS = myelodysplastic syndromes; WAGR = Wilms tumor, aniridia, genitourinary anomalies, mental retardation. | | a Adapted from Strahm et al.[76] | | b Dominant in a fraction of patients, spontaneous mutations can occur. | | Adenomatous polyposis of the colon | Colon, hepatoblastoma, intestinal cancers, stomach, thyroid cancer | APC | Dominant | | Ataxia-telangiectasia | Leukemia, lymphoma | ATM | Recessive | | Beckwith-Wiedemann syndrome | Adrenal carcinoma, hepatoblastoma, rhabdomyosarcoma, Wilms tumor | CDKN1C/NSD1 | Dominant | | Bloom syndrome | Leukemia, lymphoma, skin cancer | BLM | Recessive | | Diamond-Blackfan anemia | Colon cancer, osteogenic sarcoma, AML/MDS | RPS19and otherRPgenes | Dominant, spontaneousb | | Fanconi anemia | Gynecological tumors, leukemia, squamous cell carcinoma | FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG | Recessive | | Juvenile polyposis syndrome | Gastrointestinal tumors | SMAD4/DPC4 | Dominant | | Li-Fraumeni syndrome | Adrenocortical carcinoma, brain tumor, breast carcinoma, leukemia, osteosarcoma, soft tissue sarcoma | TP53 | Dominant | | Multiple endocrine neoplasia 1 | Pancreatic islet cell tumor, parathyroid adenoma, pituitary adenoma | MEN1 | Dominant | | Multiple endocrine neoplasia 2 | Medullary thyroid carcinoma, pheochromocytoma | RET | Dominant | | Neurofibromatosis type 1 | Neurofibroma, optic pathway glioma, peripheral nerve sheath tumor | NF1 | Dominant | | Neurofibromatosis type 2 | Vestibular schwannoma | NF2 | Dominant | | Nevoid basal cell carcinoma syndrome | Basal cell carcinoma, medulloblastoma | PTCH | Dominant | | Peutz-Jeghers syndrome | Intestinal cancers, ovarian carcinoma, pancreatic carcinoma | STK11 | Dominant | | Retinoblastoma | Osteosarcoma, retinoblastoma | RB1 | Dominant | | Tuberous sclerosis | Hamartoma, renal angiomyolipoma, renal cell carcinoma | TSC1/TSC2 | Dominant | | von Hippel-Lindau syndrome | Hemangioblastoma, pheochromocytoma, renal cell carcinoma, retinal and central nervous system tumors | VHL | Dominant | | WAGR syndrome | Gonadoblastoma, Wilms tumor | WT1 | Dominant | | Wilms tumor syndrome | Wilms tumor | WT1 | Dominant | | Xeroderma pigmentosum | Leukemia, melanoma | XPA, XPB, XPC, XPD, XPE, XPF, XPG, POLH | Recessive | Drug-metabolizing enzymes and DNA repair polymorphisms The interindividual variability in risk of SNs is more likely related to common polymorphisms in low-penetrance genes that regulate the availability of active drug metabolites or are responsible for DNA repair. Gene-environment interactions may magnify subtle functional differences resulting from genetic variations. Drug-metabolizing enzymes Metabolism of genotoxic agents occurs in two phases. - Phase I involves activation of substrates into highly reactive electrophilic intermediates that can damage DNA, a reaction principally performed by the cytochrome p450 (CYP) family of enzymes.
- Phase II enzymes (conjugation) function to inactivate genotoxic substrates. The phase II proteins comprise the glutathione S-transferase (GST), NAD(P)H:quinone oxidoreductase-1 (NQO1), and others.
The balance between the two sets of enzymes is critical to the cellular response to xenobiotics; for example, high activity of a phase I enzyme and low activity of a phase II enzyme can result in DNA damage. DNA repair polymorphisms DNA repair mechanisms protect somatic cells from mutations in tumor suppressor genes and oncogenes that can lead to cancer initiation and progression. An individual's DNA repair capacity appears to be genetically determined.[77] A number of DNA repair genes contain polymorphic variants, resulting in large interindividual variations in DNA repair capacity.[77] Evaluation of the contribution of polymorphisms influencing DNA repair to the risk of SN represents an active area of research. Screening and Follow-up for Subsequent Neoplasms Vigilant screening is important for childhood cancer survivors at risk.[78] Because of the relatively small size of the pediatric cancer survivor population and the prevalence and time to onset of therapy-related complications, undertaking clinical studies to assess the impact of screening recommendations on the morbidity and mortality associated with the late effect is not feasible. Well-conducted studies on large populations of childhood cancer survivors have provided compelling evidence linking specific therapeutic exposures and late effects. This evidence has been used by several national and international cooperative groups (Scottish Collegiate Guidelines Network, Children's Cancer and Leukaemia Group, Children's Oncology Group [COG], Dutch Children's Oncology Group) to develop consensus-based clinical practice guidelines to increase awareness and standardize the immediate care needs of medically vulnerable childhood cancer survivors.[79] All pediatric cancer survivor health screening guidelines employ a hybrid approach that is both evidence-based (utilizing established associations between therapeutic exposures and late effects to identify high-risk categories) and grounded in the collective clinical experience of experts (matching the magnitude of the risk with the intensity of the screening recommendations). The screening recommendations in these guidelines represent a statement of consensus from a panel of experts in the late effects of pediatric cancer treatment.[78,79] The COG Guidelines for malignant SNs indicate that certain high-risk populations of childhood cancer survivors merit heightened surveillance because of predisposing host, behavioral, or therapeutic factors.[78] References:
-
Mertens AC, Liu Q, Neglia JP, et al.: Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst 100 (19): 1368-79, 2008.
-
Friedman DL, Whitton J, Leisenring W, et al.: Subsequent neoplasms in 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst 102 (14): 1083-95, 2010.
-
Turcotte LM, Whitton JA, Friedman DL, et al.: Risk of Subsequent Neoplasms During the Fifth and Sixth Decades of Life in the Childhood Cancer Survivor Study Cohort. J Clin Oncol 33 (31): 3568-75, 2015.
-
Armstrong GT, Liu W, Leisenring W, et al.: Occurrence of multiple subsequent neoplasms in long-term survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 29 (22): 3056-64, 2011.
-
van Eggermond AM, Schaapveld M, Lugtenburg PJ, et al.: Risk of multiple primary malignancies following treatment of Hodgkin lymphoma. Blood 124 (3): 319-27; quiz 466, 2014.
-
Milano MT, Li H, Gail MH, et al.: Long-term survival among patients with Hodgkin's lymphoma who developed breast cancer: a population-based study. J Clin Oncol 28 (34): 5088-96, 2010.
-
Bhatia S, Yasui Y, Robison LL, et al.: High risk of subsequent neoplasms continues with extended follow-up of childhood Hodgkin's disease: report from the Late Effects Study Group. J Clin Oncol 21 (23): 4386-94, 2003.
-
Bhatia S, Sather HN, Pabustan OB, et al.: Low incidence of second neoplasms among children diagnosed with acute lymphoblastic leukemia after 1983. Blood 99 (12): 4257-64, 2002.
-
Hijiya N, Hudson MM, Lensing S, et al.: Cumulative incidence of secondary neoplasms as a first event after childhood acute lymphoblastic leukemia. JAMA 297 (11): 1207-15, 2007.
-
Bhatia S, Krailo MD, Chen Z, et al.: Therapy-related myelodysplasia and acute myeloid leukemia after Ewing sarcoma and primitive neuroectodermal tumor of bone: A report from the Children's Oncology Group. Blood 109 (1): 46-51, 2007.
-
Berger C, Trombert-Paviot B, Casagranda L, et al.: Second malignant neoplasms following childhood cancer: a study of a recent cohort (1987-2004) from the childhood cancer registry of the Rhône-Alpes region (ARCERRA) in France. Pediatr Hematol Oncol 28 (5): 364-79, 2011.
-
Nottage K, Lanctot J, Li Z, et al.: Long-term risk for subsequent leukemia after treatment for childhood cancer: a report from the Childhood Cancer Survivor Study. Blood 117 (23): 6315-8, 2011.
-
Tefferi A, Vardiman JW: Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia 22 (1): 14-22, 2008.
-
Thirman MJ, Larson RA: Therapy-related myeloid leukemia. Hematol Oncol Clin North Am 10 (2): 293-320, 1996.
-
Pedersen-Bjergaard J, Philip P: Balanced translocations involving chromosome bands 11q23 and 21q22 are highly characteristic of myelodysplasia and leukemia following therapy with cytostatic agents targeting at DNA-topoisomerase II. Blood 78 (4): 1147-8, 1991.
-
Bassal M, Mertens AC, Taylor L, et al.: Risk of selected subsequent carcinomas in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 24 (3): 476-83, 2006.
-
Neglia JP, Robison LL, Stovall M, et al.: New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst 98 (21): 1528-37, 2006.
-
Perkins JL, Liu Y, Mitby PA, et al.: Nonmelanoma skin cancer in survivors of childhood and adolescent cancer: a report from the childhood cancer survivor study. J Clin Oncol 23 (16): 3733-41, 2005.
-
Boukheris H, Stovall M, Gilbert ES, et al.: Risk of salivary gland cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Int J Radiat Oncol Biol Phys 85 (3): 776-83, 2013.
-
Chowdhry AK, McHugh C, Fung C, et al.: Second primary head and neck cancer after Hodgkin lymphoma: a population-based study of 44,879 survivors of Hodgkin lymphoma. Cancer 121 (9): 1436-45, 2015.
-
Ronckers CM, Sigurdson AJ, Stovall M, et al.: Thyroid cancer in childhood cancer survivors: a detailed evaluation of radiation dose response and its modifiers. Radiat Res 166 (4): 618-28, 2006.
-
Fidler MM, Frobisher C, Guha J, et al.: Long-term adverse outcomes in survivors of childhood bone sarcoma: the British Childhood Cancer Survivor Study. Br J Cancer 112 (12): 1857-65, 2015.
-
Majhail NS, Brazauskas R, Rizzo JD, et al.: Secondary solid cancers after allogeneic hematopoietic cell transplantation using busulfan-cyclophosphamide conditioning. Blood 117 (1): 316-22, 2011.
-
Bhatia S, Sklar C: Second cancers in survivors of childhood cancer. Nat Rev Cancer 2 (2): 124-32, 2002.
-
Kenney LB, Yasui Y, Inskip PD, et al.: Breast cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Intern Med 141 (8): 590-7, 2004.
-
Travis LB, Hill D, Dores GM, et al.: Cumulative absolute breast cancer risk for young women treated for Hodgkin lymphoma. J Natl Cancer Inst 97 (19): 1428-37, 2005.
-
O'Brien MM, Donaldson SS, Balise RR, et al.: Second malignant neoplasms in survivors of pediatric Hodgkin's lymphoma treated with low-dose radiation and chemotherapy. J Clin Oncol 28 (7): 1232-9, 2010.
-
Inskip PD, Robison LL, Stovall M, et al.: Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol 27 (24): 3901-7, 2009.
-
Dores GM, Anderson WF, Beane Freeman LE, et al.: Risk of breast cancer according to clinicopathologic features among long-term survivors of Hodgkin's lymphoma treated with radiotherapy. Br J Cancer 103 (7): 1081-4, 2010.
-
Horst KC, Hancock SL, Ognibene G, et al.: Histologic subtypes of breast cancer following radiotherapy for Hodgkin lymphoma. Ann Oncol 25 (4): 848-51, 2014.
-
Castiglioni F, Terenziani M, Carcangiu ML, et al.: Radiation effects on development of HER2-positive breast carcinomas. Clin Cancer Res 13 (1): 46-51, 2007.
-
Gaffney DK, Hemmersmeier J, Holden J, et al.: Breast cancer after mantle irradiation for Hodgkin's disease: correlation of clinical, pathologic, and molecular features including loss of heterozygosity at BRCA1 and BRCA2. Int J Radiat Oncol Biol Phys 49 (2): 539-46, 2001.
-
Janov AJ, Tulecke M, O'Neill A, et al.: Clinical and pathologic features of breast cancers in women treated for Hodgkin's disease: a case-control study. Breast J 7 (1): 46-52, 2001 Jan-Feb.
-
Travis LB, Hill DA, Dores GM, et al.: Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA 290 (4): 465-75, 2003.
-
van Leeuwen FE, Klokman WJ, Stovall M, et al.: Roles of radiation dose, chemotherapy, and hormonal factors in breast cancer following Hodgkin's disease. J Natl Cancer Inst 95 (13): 971-80, 2003.
-
Moskowitz CS, Chou JF, Wolden SL, et al.: Breast cancer after chest radiation therapy for childhood cancer. J Clin Oncol 32 (21): 2217-23, 2014.
-
Lange JM, Takashima JR, Peterson SM, et al.: Breast cancer in female survivors of Wilms tumor: a report from the national Wilms tumor late effects study. Cancer 120 (23): 3722-30, 2014.
-
Henderson TO, Moskowitz CS, Chou JF, et al.: Breast Cancer Risk in Childhood Cancer Survivors Without a History of Chest Radiotherapy: A Report From the Childhood Cancer Survivor Study. J Clin Oncol 34 (9): 910-8, 2016.
-
van Santen HM, Tytgat GA, van de Wetering MD, et al.: Differentiated thyroid carcinoma after 131I-MIBG treatment for neuroblastoma during childhood: description of the first two cases. Thyroid 22 (6): 643-6, 2012.
-
Sklar C, Whitton J, Mertens A, et al.: Abnormalities of the thyroid in survivors of Hodgkin's disease: data from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 85 (9): 3227-32, 2000.
-
Bhatti P, Veiga LH, Ronckers CM, et al.: Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: an update from the childhood cancer survivor study. Radiat Res 174 (6): 741-52, 2010.
-
Michaelson EM, Chen YH, Silver B, et al.: Thyroid malignancies in survivors of Hodgkin lymphoma. Int J Radiat Oncol Biol Phys 88 (3): 636-41, 2014.
-
Sigurdson AJ, Ronckers CM, Mertens AC, et al.: Primary thyroid cancer after a first tumour in childhood (the Childhood Cancer Survivor Study): a nested case-control study. Lancet 365 (9476): 2014-23, 2005 Jun 11-17.
-
Neglia JP, Friedman DL, Yasui Y, et al.: Second malignant neoplasms in five-year survivors of childhood cancer: childhood cancer survivor study. J Natl Cancer Inst 93 (8): 618-29, 2001.
-
Bowers DC, Nathan PC, Constine L, et al.: Subsequent neoplasms of the CNS among survivors of childhood cancer: a systematic review. Lancet Oncol 14 (8): e321-8, 2013.
-
Taylor AJ, Little MP, Winter DL, et al.: Population-based risks of CNS tumors in survivors of childhood cancer: the British Childhood Cancer Survivor Study. J Clin Oncol 28 (36): 5287-93, 2010.
-
Faraci M, Morana G, Bagnasco F, et al.: Magnetic resonance imaging in childhood leukemia survivors treated with cranial radiotherapy: a cross sectional, single center study. Pediatr Blood Cancer 57 (2): 240-6, 2011.
-
Vinchon M, Leblond P, Caron S, et al.: Radiation-induced tumors in children irradiated for brain tumor: a longitudinal study. Childs Nerv Syst 27 (3): 445-53, 2011.
-
Koike T, Yanagimachi N, Ishiguro H, et al.: High incidence of radiation-induced cavernous hemangioma in long-term survivors who underwent hematopoietic stem cell transplantation with radiation therapy during childhood or adolescence. Biol Blood Marrow Transplant 18 (7): 1090-8, 2012.
-
Tucker MA, D'Angio GJ, Boice JD Jr, et al.: Bone sarcomas linked to radiotherapy and chemotherapy in children. N Engl J Med 317 (10): 588-93, 1987.
-
Hawkins MM, Wilson LM, Burton HS, et al.: Radiotherapy, alkylating agents, and risk of bone cancer after childhood cancer. J Natl Cancer Inst 88 (5): 270-8, 1996.
-
Wong JR, Morton LM, Tucker MA, et al.: Risk of subsequent malignant neoplasms in long-term hereditary retinoblastoma survivors after chemotherapy and radiotherapy. J Clin Oncol 32 (29): 3284-90, 2014.
-
Schwartz B, Benadjaoud MA, Cléro E, et al.: Risk of second bone sarcoma following childhood cancer: role of radiation therapy treatment. Radiat Environ Biophys 53 (2): 381-90, 2014.
-
Henderson TO, Whitton J, Stovall M, et al.: Secondary sarcomas in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst 99 (4): 300-8, 2007.
-
Shinohara ET, DeWees T, Perkins SM: Subsequent malignancies and their effect on survival in patients with retinoblastoma. Pediatr Blood Cancer 61 (1): 116-9, 2014.
-
MacCarthy A, Bayne AM, Brownbill PA, et al.: Second and subsequent tumours among 1927 retinoblastoma patients diagnosed in Britain 1951-2004. Br J Cancer 108 (12): 2455-63, 2013.
-
Yu CL, Tucker MA, Abramson DH, et al.: Cause-specific mortality in long-term survivors of retinoblastoma. J Natl Cancer Inst 101 (8): 581-91, 2009.
-
Henderson TO, Rajaraman P, Stovall M, et al.: Risk factors associated with secondary sarcomas in childhood cancer survivors: a report from the childhood cancer survivor study. Int J Radiat Oncol Biol Phys 84 (1): 224-30, 2012.
-
Daniëls LA, Krol AD, Schaapveld M, et al.: Long-term risk of secondary skin cancers after radiation therapy for Hodgkin's lymphoma. Radiother Oncol 109 (1): 140-5, 2013.
-
Watt TC, Inskip PD, Stratton K, et al.: Radiation-related risk of basal cell carcinoma: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst 104 (16): 1240-50, 2012.
-
Braam KI, Overbeek A, Kaspers GJ, et al.: Malignant melanoma as second malignant neoplasm in long-term childhood cancer survivors: a systematic review. Pediatr Blood Cancer 58 (5): 665-74, 2012.
-
Pappo AS, Armstrong GT, Liu W, et al.: Melanoma as a subsequent neoplasm in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Pediatr Blood Cancer 60 (3): 461-6, 2013.
-
van Leeuwen FE, Klokman WJ, Stovall M, et al.: Roles of radiotherapy and smoking in lung cancer following Hodgkin's disease. J Natl Cancer Inst 87 (20): 1530-7, 1995.
-
Tukenova M, Diallo I, Anderson H, et al.: Second malignant neoplasms in digestive organs after childhood cancer: a cohort-nested case-control study. Int J Radiat Oncol Biol Phys 82 (3): e383-90, 2012.
-
Henderson TO, Oeffinger KC, Whitton J, et al.: Secondary gastrointestinal cancer in childhood cancer survivors: a cohort study. Ann Intern Med 156 (11): 757-66, W-260, 2012.
-
Nottage K, McFarlane J, Krasin MJ, et al.: Secondary colorectal carcinoma after childhood cancer. J Clin Oncol 30 (20): 2552-8, 2012.
-
Wilson CL, Ness KK, Neglia JP, et al.: Renal carcinoma after childhood cancer: a report from the childhood cancer survivor study. J Natl Cancer Inst 105 (7): 504-8, 2013.
-
Reulen RC, Frobisher C, Winter DL, et al.: Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA 305 (22): 2311-9, 2011.
-
de Vathaire F, Scwhartz B, El-Fayech C, et al.: Risk of a Second Kidney Carcinoma Following Childhood Cancer: Role of Chemotherapy and Radiation Dose to Kidneys. J Urol 194 (5): 1390-5, 2015.
-
Fleitz JM, Wootton-Gorges SL, Wyatt-Ashmead J, et al.: Renal cell carcinoma in long-term survivors of advanced stage neuroblastoma in early childhood. Pediatr Radiol 33 (8): 540-5, 2003.
-
Hedgepeth RC, Zhou M, Ross J: Rapid development of metastatic Xp11 translocation renal cell carcinoma in a girl treated for neuroblastoma. J Pediatr Hematol Oncol 31 (8): 602-4, 2009.
-
Argani P, Laé M, Ballard ET, et al.: Translocation carcinomas of the kidney after chemotherapy in childhood. J Clin Oncol 24 (10): 1529-34, 2006.
-
Archer NM, Amorim RP, Naves R, et al.: An Increased Risk of Second Malignant Neoplasms After Rhabdomyosarcoma: Population-Based Evidence for a Cancer Predisposition Syndrome? Pediatr Blood Cancer 63 (2): 196-201, 2016.
-
Andersson A, Enblad G, Tavelin B, et al.: Family history of cancer as a risk factor for second malignancies after Hodgkin's lymphoma. Br J Cancer 98 (5): 1001-5, 2008.
-
Hisada M, Garber JE, Fung CY, et al.: Multiple primary cancers in families with Li-Fraumeni syndrome. J Natl Cancer Inst 90 (8): 606-11, 1998.
-
Strahm B, Malkin D: Hereditary cancer predisposition in children: genetic basis and clinical implications. Int J Cancer 119 (9): 2001-6, 2006.
-
Collins A, Harrington V: Repair of oxidative DNA damage: assessing its contribution to cancer prevention. Mutagenesis 17 (6): 489-93, 2002.
-
Landier W, Bhatia S, Eshelman DA, et al.: Development of risk-based guidelines for pediatric cancer survivors: the Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol 22 (24): 4979-90, 2004.
-
Kremer LC, Mulder RL, Oeffinger KC, et al.: A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer 60 (4): 543-9, 2013.
-
Diller L, Medeiros Nancarrow C, Shaffer K, et al.: Breast cancer screening in women previously treated for Hodgkin's disease: a prospective cohort study. J Clin Oncol 20 (8): 2085-91, 2002.
-
Mulder RL, Kremer LC, Hudson MM, et al.: Recommendations for breast cancer surveillance for female survivors of childhood, adolescent, and young adult cancer given chest radiation: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol 14 (13): e621-9, 2013.
-
Kriege M, Brekelmans CT, Boetes C, et al.: Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med 351 (5): 427-37, 2004.
-
Leach MO, Boggis CR, Dixon AK, et al.: Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS). Lancet 365 (9473): 1769-78, 2005 May 21-27.
-
Tieu MT, Cigsar C, Ahmed S, et al.: Breast cancer detection among young survivors of pediatric Hodgkin lymphoma with screening magnetic resonance imaging. Cancer 120 (16): 2507-13, 2014.
-
Saslow D, Boetes C, Burke W, et al.: American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 57 (2): 75-89, 2007 Mar-Apr.
-
Berrington de Gonzalez A, Berg CD, Visvanathan K, et al.: Estimated risk of radiation-induced breast cancer from mammographic screening for young BRCA mutation carriers. J Natl Cancer Inst 101 (3): 205-9, 2009.
-
Young KC, Burch A, Oduko JM: Radiation doses received in the UK Breast Screening Programme in 2001 and 2002. Br J Radiol 78 (927): 207-18, 2005.
-
Spelic DC: Updated Trends in Mammography Dose and Image Quality. Silver Spring, Md: U.S. Food and Drug Administration, 2006. Available online. Last accessed March 31, 2016.
Late Effects of the Cardiovascular SystemCardiovascular disease, after recurrence of the original cancer and development of second primary cancers, has been reported to be the leading cause of premature mortality among long-term childhood cancer survivors.[1,2,3,4,5] Evidence supports the excess risk of premature cardiovascular mortality as follows: - Among more than 20,000 North American 5-year survivors of childhood cancer (in the Childhood Cancer Survivor Study [CCSS]) treated from 1970 to 1986, participants had a standardized mortality ratio of 7.0 (95% confidence interval [CI], 5.9-8.2) for cardiac mortality, which translated to 0.36 excess deaths per 1,000 person-years.[1]
- All-cause circulatory disease was associated with an absolute excess risk of 3.4% (95% CI, 2.8-4.2) among nearly 18,000 5-year survivors in the British Childhood Cancer Survivor Study who were diagnosed with cancer between 1950 and 1991. Individual standardized mortality ratios for cardiac, cerebrovascular, and other circulatory diseases ranged from 3.5 to 5.2.[2]
By age 45 years, the overall cumulative incidence of severe, life-threatening, or fatal cardiac events has been reported to be approximately 5% for coronary artery disease and heart failure separately and 1% to 2% for valve disorders and arrhythmias.[6] Compared with siblings, 5-year survivors had relative risks (RRs) approaching, if not exceeding, tenfold for heart failure, coronary artery disease, and cerebrovascular disease.[7] The burden of subclinical disease is likely much greater.[8] The specific late effects covered in this section include the following: - Cardiomyopathy/heart failure.
- Ischemic heart disease.
- Pericardial heart disease.
- Valve disease.
- Conduction disorders.
- Cerebrovascular disease.
The section will also briefly discuss the influence of related conditions such as hypertension, dyslipidemia, and diabetes in relation to these late effects, but not directly review in detail those conditions as a consequence of childhood cancer treatment. A comprehensive review on long-term cardiovascular toxicity in childhood and young adult survivors of cancer, issued by the American Heart Association, has been published.[5] Overall, there has been a wealth of studies focused on the topic of cardiac events among childhood cancer survivors. In addition to many smaller studies not covered in detail here, the literature includes very large cohort studies that are either hospital based,[6,8,9,10,11,12] clinical trial based,[13,14] or population based,[2,4] many with up to several decades of follow-up. However, even with decades of follow-up, the average age of these populations may still be relatively young (middle or young adulthood). And while the risk of serious cardiovascular outcomes may be very high relative to the age-matched general population, the absolute risk often remains low, limiting the power of many studies. Among the very large studies featuring thousands of survivors, the main limitation has been inadequate ability to clinically ascertain late cardiovascular complications, with a greater reliance on either administrative records (e.g., death registries) and/or self-report or proxy-report. While each study design has some inherent biases, the overall literature, based on a combination of self-reported outcomes, clinical ascertainment, and administrative data sources, is robust in concluding that certain cancer-related exposures predispose survivors toward a significantly greater risk of cardiovascular morbidity and mortality. Although late effects research often lags behind changes in contemporary therapy, many therapies linked to cardiovascular late effects remain in common use today.[15,16] Ongoing research will be important to ensure that newer targeted agents being introduced today do not result in unexpected cardiovascular effects.[17] Results of selected cohort studies describing the rates of cardiovascular outcomes include the following: - A multicenter French cohort of 3,162 5-year survivors treated between 1942 and 1986 were monitored for a median of 26 years. The cumulative incidence of any cardiac disease (ischemic heart disease, heart failure, arrhythmia, or valve and pericardial diseases) by age 40 years was 11% (7% if restricted to those that warranted medical intervention). Risk increased with higher anthracycline and radiation doses, particularly anthracycline doses of 250 mg/m2 or more and heart radiation doses of 15 Gy or higher. A significant interaction was identified between radiation dose, anthracycline exposure, and attained age.[12]
- In a Dutch hospital-based cohort of 1,362 5-year childhood cancer survivors (median attained age, 29.1 years; median follow-up time from diagnosis, 22.2 years), the 30-year cause-specific cumulative incidence of symptomatic cardiac events (congestive heart failure, cardiac ischemia, valve disease, arrhythmia, and/or pericarditis) was significantly increased after treatment with both anthracyclines and cardiac radiation (12.6%; 95% CI, 4.3-10.3), anthracyclines alone (7.3%; 95% CI, 3.8-10.7), and cardiac radiation alone (4.0%; 95% CI, 0.5-7.4) compared with other treatments.[11]
- A report from the CCSS that featured over 14,000 5-year survivors examined detailed dose-response to both radiation therapy and chemotherapy (anthracycline) in relation to self-reported (or death caused by) myocardial infarction, congestive heart failure, pericardial disease, and valvular abnormalities. Cardiac radiation doses of 15 Gy or higher were associated with substantially greater risk compared with the risk seen in nonirradiated survivors, while anthracycline doses of 250 mg/m2 or more were associated with a substantially increased risk of congestive heart failure, pericardial disease, and valvular abnormalities, independent of radiation exposure. Overall, the cumulative incidence of adverse cardiac outcomes continued to rise more than 30 years after original cancer diagnosis.[10]
- A follow-up study from the CCSS demonstrated that the cumulative incidence of these serious cardiac events continued to increase beyond age 45 years. Furthermore, the risk of these events was potentiated (i.e., beyond what would be expected by an additive model) by the presence of concurrent, but potentially modifiable, conditions such as obesity, dyslipidemia, diabetes, and, particularly, hypertension. Hypertension was independently associated with all serious cardiac outcomes (RRs, 6-fold to 19-fold), even after adjustment for anthracycline use and chest irradiation.[6]
- Using data from four large, well-annotated childhood cancer survivor cohorts (CCSS, National Wilms Tumor Study Group, the Netherlands, and St. Jude Children's Research Hospital [SJCRH]), a heart failure risk calculator based on readily available demographic and treatment characteristics has been created and validated, which may provide more individualized clinical heart failure risk estimation for 5-year survivors of childhood cancer who have recently completed therapy and up through age 40 years. One limitation of this estimator is that because of the young age of participants at the time of baseline prediction (5-year survival), information on conventional cardiovascular conditions such as hypertension, dyslipidemia, or diabetes could not be incorporated.[18]
- Of 670 survivors of Hodgkin lymphoma (HL) who were treated at SJCRH and have lived 10 or more years, 348 patients were clinically assessed in the St. Jude Lifetime Cohort Study. At age 50 years, the cumulative incidence of those survivors experiencing at least one grade 3 to grade 5 cardiovascular condition was 45.5% (95% CI, 36.6-54.3), compared with 15.7% (95% CI, 7.0-24.4) in community controls. Myocardial infarction and structural heart defects were the major contributors to the excess grade 3 to grade 5 cumulative burden in survivors.[19]
Treatment Risk Factors Chemotherapy (in particular, anthracyclines and anthraquinones) along with radiation therapy both independently and in combination, increase the risk of cardiovascular disease in survivors of childhood cancer and are considered to be the most important risk factors contributing to premature cardiovascular disease in this population (refer to Figure 2).[11]
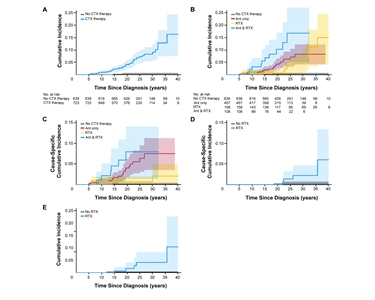
Figure 2. (A, B) Marginal (Kaplan-Meier) and (C-E) cause-specific (competing risk) cumulative incidence of cardiac events (CEs) in childhood cancer survivors stratified according to different treatment groups. (A) Marginal cumulative incidence for all CEs, stratified according to potential cardiotoxic (CTX) therapy or no CTX therapy, log-rank P < .001. (B) Marginal cumulative incidence for all CEs, stratified according to different CTX therapies, log-rank P < .001. (C) Cause-specific cumulative incidence for congestive heart failure, stratified according to different treatment groups, log-rank P < .001. (D) Cause-specific cumulative incidence for cardiac ischemia, stratified according to cardiac irradiation (RTX) or no RTX, log-rank P = .01. (E) Cause-specific cumulative incidence for valvular disease, stratified according to RTX or no RTX, log-rank P < .001. The shaded colorized background areas refer to the 95% CIs. Ant, anthracycline. Helena J. van der Pal, Elvira C. van Dalen, Evelien van Delden, Irma W. van Dijk, Wouter E. Kok, Ronald B. Geskus, Elske Sieswerda, Foppe Oldenburger, Caro C. Koning, Flora E. van Leeuwen, Huib N. Caron, Leontien C. Kremer, High Risk of Symptomatic Cardiac Events in Childhood Cancer Survivors, Journal of Clinical Oncology, volume 30, issue 13, pages 1429-1437. Reprinted with permission. © (2012) American Society of Clinical Oncology. All rights reserved.
Anthracyclines and related agents Anthracyclines (e.g., doxorubicin, daunorubicin, idarubicin, and epirubicin) and anthraquinones (e.g., mitoxantrone) are known to directly injure cardiomyocytes through the formation of reactive oxygen species and inducing mitochondrial apoptosis.[5,20] The downstream results of cell death are changes in heart structure, including wall thinning, which leads to ventricular overload and pathologic remodeling that, over time, leads to dysfunction and eventual clinical heart failure.[21,22,23,24] Risk factors for anthracycline-related cardiomyopathy include the following:[25] - Cumulative dose, particularly greater than 250 mg/m2 to 300 mg/m2.
- Younger age at time of exposure, particularly children younger than 5 years.
- Increased time from exposure.
Among these factors, cumulative dose appears to be the most significant (refer to Figure 3).[9] While it is not completely certain whether there is a truly safe lower dose threshold, doses in excess of 250 mg/m2 to 300 mg/m2 have been associated with a substantially increased risk of cardiomyopathy, with cumulative incidences exceeding 5% after 20 years of follow-up, and in some subgroups, reaching or exceeding 10% cumulative incidence by age 40 years.[9,10,18,22,24] Concurrent chest or heart radiation therapy also further increases risk of cardiomyopathy,[11,12,18] as does the presence of other cardiometabolic traits such as hypertension.[6,26] While development of clinical heart failure can occur within a few years after anthracycline exposure, in most survivors, even those who received very high doses, clinical manifestations may not occur for decades.
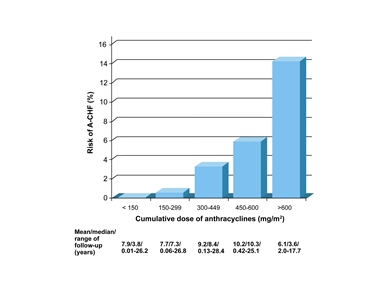
Figure 3. Risk of anthracycline-induced clinical heart failure (A-CHF) according to cumulative anthracycline dose. Reprinted from European Journal of Cancer, Volume 42, Elvira C. van Dalen, Helena J.H. van der Pal, Wouter E.M. Kok, Huib N. Caron, Leontien C.M. Kremer, Clinical heart failure in a cohort of children treated with anthracyclines: A long-term follow-up study, Pages 3191-3198, Copyright (2006), with permission from Elsevier.
Anthracycline Dose Equivalency It remains unclear how best to add together doses of different anthracycline agents. A variety of anthracycline equivalence formulas (in relation to doxorubicin) have been used; however, they are largely based on hematologic toxicity equivalence, and may not necessarily be the same for cardiac toxicity.[18,27,28] Most pediatric professional societies and groups have generally considered daunorubicin equivalent, or near equivalent, to doxorubicin, although historically lower ratios have been proposed as well.[29] A recent large analysis of over 15,000 childhood cancer survivors who were monitored to age 40 years found that daunorubicin may be significantly less cardiotoxic than doxorubicin (equivalence ratio, 0.5 [95% CI, 0.2-0.7]).[30] Other agents such as idarubicin, epirubicin, and mitoxantrone (an anthraquinone) were designed to reduce cardiac toxicity while maintaining similar antitumor effect, although data supporting this are primarily limited to adult cancer patients.[31] Similarly, data on whether liposomal formulations of anthracyclines reduce cardiac toxicity in children also are limited.[31] Anthracycline Cardioprotection In addition to new, less cardiotoxic agents and liposomal formulations, other cardioprotective strategies that have been explored include the following: - Prolonged infusion time. Prolonged infusion time has been associated with reduced heart failure in adult patients but not in children.[32,33]
- Concurrent administration of cardioprotectants. A variety of agents have been tested as cardioprotectants (amifostine, acetylcysteine, calcium channel blockers, carvedilol, coenzyme Q10, and L-carnitine), but none have been definitively shown to be beneficial and are not considered standard of care.[34,35] There are more data for dexrazoxane as a cardioprotectant, but again, mainly in adult cancer patients, for whom it is approved by the U.S. Food and Drug Administration for women with metastatic breast cancer who have received 300 mg/m2 of anthracyclines and who may benefit from further anthracycline-based therapy.[34] Pediatric data show that dexrazoxane may ameliorate some markers of early cardiac toxicity up to 5 years after therapy.[36,37,38,39] Dexrazoxane may be associated with an increased risk of acute toxicities in some regimens, however.[40] While these data suggest that dexrazoxane does protect the heart in the short term, there are not yet long-term data showing the impact of dexrazoxane on cardiac health.
Radiation therapy While anthracyclines directly damage cardiomyocytes, radiation therapy primarily affects the fine vasculature of affected organs.[5] Late effects of radiation therapy to the heart specifically include the following: - Delayed pericarditis, which can present abruptly or as a chronic pericardial effusion.
- Pancarditis, which includes pericardial and myocardial fibrosis, with or without endocardial fibroelastosis.
- Cardiomyopathy (in the absence of significant pericardial disease), which can occur even without anthracycline exposure.
- Ischemic heart disease.
- Functional valve injury, often aortic.
- Conduction defects.
These cardiac late effects are related to total radiation dose, individual radiation fraction size, and the volume of the heart that is exposed. Various studies have demonstrated a substantially increased risk of these outcomes with higher radiation doses, particularly doses to the heart exceeding 35 Gy (refer to Figure 4).[10,11,12,14,41,42] At higher radiation doses, rates of heart failure, pericardial disease, and valvular disease have been reported to exceed 10% after 20 to 30 years. However, even doses as low as 5 Gy have been associated with an increased risk of cardiac mortality and other serious cardiac morbidity, with possibly an exponential dose relationship.[3,11] Similar to anthracyclines, manifestation of these late effects may take years, if not decades, to present. Finally, patients who were exposed to both radiation therapy affecting the cardiovascular system and cardiotoxic chemotherapies are at even greater risk of late cardiovascular outcomes.[12]
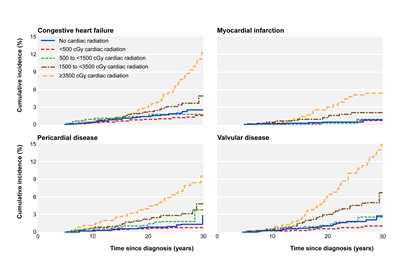
Figure 4. Cumulative incidence of cardiac disorders among childhood cancer survivors by average cardiac radiation dose. BMJ 2009; 339:b4606. © 2009 by British Medical Journal Publishing Group.
Cerebrovascular disease after radiation therapy exposure is another potential late effect for survivors. While brain tumor survivors have had traditionally the greatest risk, other survivors exposed to cranial radiation (≥18 Gy) and neck radiation (≥40 Gy), such as leukemia and lymphoma survivors, have also been reported to be at increased risk.[43,44,45] In lymphoma survivors who only received chest and/or neck radiation therapy, cerebrovascular disease is thought to be caused by large-vessel atherosclerosis and cardiac embolism.[44] As with cardiac outcomes, risk increases with cumulative dose received. One study (N = 325) reported that the stroke hazard increased by 5% (hazard ratio [HR], 1.05; 95% CI, 1.01-1.09; P = .02), with each 1 Gy increase in the radiation dose, leading to a cumulative incidence of 2% for the first stroke after 5 years and 4% after 10 years.[46] Survivors who experienced stroke were then at significantly greater risk of experiencing recurrent strokes. Results of selected studies describing prevalence of and risk factors for cerebrovascular accident (CVA)/vascular disease in childhood cancer survivors include the following: - In a multicenter retrospective Dutch study, among 2,201 5-year survivors of HL diagnosed before age 51 years (25% pediatric-aged patients), with a median follow-up of 18 years, 96 patients developed cerebrovascular disease (CVA and transient ischemic attacks [TIA]). Most ischemic events were from large-artery atherosclerosis (36%) or cardiac embolism (24%). The cumulative incidence of ischemic CVA or TIA 30 years after lymphoma treatment was 7%. The overall standardized incidence ratio (SIR) was 2.2 for CVA and 3.1 for TIA. However, SIR estimates appeared to be greater among childhood cancer survivors, with SIRs of 3.8 for CVA and 7.6 for TIA. Irradiation to the neck and mediastinum was an independent risk factor for ischemic cerebrovascular disease (HR, 2.5; 95% CI, 1.1-5.6) versus no radiation therapy. Treatment with chemotherapy was not associated with increased risk. Finally, hypertension, diabetes mellitus, and hypercholesterolemia were associated with the occurrence of ischemic cerebrovascular disease.[44]
- French investigators observed a significant association between radiation dose to the brain and long-term cerebrovascular mortality among 4,227 5-year childhood cancer survivors (median follow-up, 29 years). Survivors who received more than 50 Gy to the prepontine cistern had an HR of 17.8 (95% CI, 4.4-73) for death from cerebrovascular disease, compared with those who had not received radiation therapy or who had received less than 0.1 Gy in the prepontine cistern region.[45]
- A retrospective, single-center, cohort study of 325 survivors of pediatric cancer treated with cranial irradiation or cervical irradiation determined that cranial irradiation put survivors at a high risk of first and recurrent strokes. The cumulative incidence of first stroke was 4% (95% CI, 2.0-8.4) at 10 years after radiation therapy. The stroke hazard increased by 5% (HR, 1.05; 95% CI, 1.01-1.09; P = .02) with each 1 Gy increase in the radiation dose. The cumulative incidence of recurrent stroke was 38% (95% CI, 17-69) at 5 years and 59% (95% CI, 27-92) at 10 years after the first stroke.[46]
- CCSS investigators evaluated the rates and predictors of recurrent stroke among participants who reported a first stroke. Among responding participants (329 of 443), 271 confirmed a first stroke (at median age, 19 years) and 70 reported a second stroke (at median age, 32 years). Independent predictors of recurrent stroke included treatment with a cranial radiation therapy dose of 50 Gy or higher (vs. no cranial radiation therapy), history of hypertension, and age 40 years or older at first stroke (vs. age 0-17 years). The 10-year cumulative incidence of late recurrent stroke was 21% overall, and 33% for those treated with 50 Gy or higher of cranial radiation therapy.[47]
Conventional cardiovascular conditions Various cancer treatment exposures may also directly or indirectly influence the development of hypertension, diabetes mellitus, and dyslipidemia.[5] These conditions remain important among cancer survivors, as they do in the general population, in that they are independent risk factors in the development of cardiomyopathy, ischemic heart disease, and cerebrovascular disease.[6,44,48,49,50] Childhood cancer survivors should be closely screened for the development of these conditions because they represent potentially modifiable targets for intervention. This includes being aware of related conditions such as obesity and various endocrinopathies (e.g., hypothyroidism, hypogonadism, growth hormone deficiency) that may be more common among subsets of childhood cancer survivors, and if these conditions are untreated/uncontrolled, they may be associated with a metabolic profile that increases cardiovascular risk.[8,51] Other Risk Factors Some, but not all, studies suggest that female gender may be associated with a greater risk of anthracycline-related cardiomyopathy.[5] In addition, there is emerging evidence that genetic factors, such as single nucleotide polymorphisms in genes regulating drug metabolism and distribution, could explain the heterogeneity in susceptibility to anthracycline-mediated cardiac injury.[52,53,54,55,56,57] However, these genetic findings still require additional validation before being incorporated into any clinical screening algorithm.[58] Knowledge Deficits While much knowledge has been gained over the past 20 years in better understanding the long-term burden and risk factors for cardiovascular disease among childhood cancer survivors, many areas of inquiry remain, and include the following: - Radiation may have both direct and indirect effects on vascular endothelium, contributing to vascular damage beyond the primary radiation field.[59]
- The long-term effects of lower radiation doses, particularly in light of newer technology that allows radiation oncologists to reduce the dose to critical organs outside of the tumor field, remain to be determined.[60]
- The long-term effects of many newer anticancer agents that are based on molecular targets remains unclear, although some of them are known to have shorter-term cardiac toxicity.[17]
- The efficacy of cardioprotective strategies, including the use of alternative anthracycline formulations that appear promising in adults, requires further study in children.[35]
Screening, Surveillance, and Counseling Various national groups, including the National Institutes of Health-sponsored COG (refer to Table 2), have published recommendations regarding screening and surveillance for cardiovascular and other late effects among childhood cancer survivors.[61,62,63,64,65] Professional groups (both pediatric and adult) have developed evidence-based health surveillance recommendations and have identified knowledge deficits to help guide future studies.[25,66] Adult oncology professional and national groups have also issued recommendations related to cardiac toxicity monitoring.[67] At this point, there is no clear evidence (at least through age 50 years or 30 to 40 years posttreatment) that there is a plateau in risk that occurs after a certain time among survivors exposed to cancer treatments associated with cardiovascular late effects.[3,4,10,11,43,68] Thus, some form of life-long surveillance is recommended, even if the cost-effectiveness of certain screening strategies remains unclear.[25,69,70,71] However, a growing amount of literature is beginning to establish the yield from these screening studies, which will help inform future guidelines.[8,72,73,74] In these studies, for example, among adult-aged survivors of childhood cancer, evidence for cardiomyopathy on the basis of echocardiographic changes was found in approximately 6% of at-risk survivors. Overall, in a cohort of more than 1,000 survivors (median age, 32 years), nearly 60% of screened at-risk survivors had some clinically ascertained cardiac abnormality identified.[8] Given the growing evidence that conventional cardiovascular conditions such as hypertension, dyslipidemia, and diabetes substantially increase the risk of more serious cardiovascular disease among survivors, clinicians should carefully consider baseline and follow-up screening and treatment of these comorbid conditions that impact cardiovascular health.[6,44,48,49] There is also emerging evidence that adoption of healthier lifestyle factors may decrease future cardiovascular morbidity in at-risk survivors.[75] Thus, similar to the general population, survivors are counseled about maintaining a healthy weight, participating in regular physical activity, adhering to a heart-healthy diet, and abstaining from smoking. In addition to releasing a comprehensive, publically available (online) set of guidelines, the COG has also put together a series of handouts on cardiovascular and related topics, including lifestyle choices written for a lay audience, available on the same website. Table 2. Cardiovascular Late Effectsa,b| Predisposing Therapy | Potential Cardiovascular Effects | Health Screening |
|---|
| a The Children's Oncology Group (COG) guidelines also cover other conditions that may influence cardiovascular risk also exist, such as obesity and diabetes mellitus/impaired glucose metabolism. | | b Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Any anthracycline and/or any radiation to the heart | Cardiac toxicity (arrhythmia, cardiomyopathy/heart failure, pericardial disease, valve disease, ischemic heart disease) | Yearly medical history and physical exam | | Electrocardiogram at entry into long-term follow-up | | Echocardiogram at entry into long-term follow-up, periodically repeat based on previous exposures and other risk factors | | Radiation to the area (≥40 Gy) | Carotid and/or subclavian artery disease | Yearly medical history and physical exam; consider Doppler ultrasound 10 years after exposure | | Radiation to the brain/cranium (≥18 Gy) | Cerebrovascular disease (cavernomas, Moyamoya, occlusive cerebral vasculopathy, stroke) | Yearly medical history and physical exam | | Radiation to the abdomen | Diabetes | Diabetes screen every 2 years | | Total-body irradiation | Dyslipidemia; diabetes | Fasting lipid profile and diabetes screen every 2 years | | Heavy metals (carboplatin, cisplatin), ifosfamide, and methotrexate exposure; radiation to the kidneys; hematopoietic cell transplantation; nephrectomy | Hypertension (as a consequence of renal toxicity) | Yearly blood pressure and urinalysis; renal function laboratory studies at entry into long-term follow-up | References:
-
Mertens AC, Liu Q, Neglia JP, et al.: Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst 100 (19): 1368-79, 2008.
-
Reulen RC, Winter DL, Frobisher C, et al.: Long-term cause-specific mortality among survivors of childhood cancer. JAMA 304 (2): 172-9, 2010.
-
Tukenova M, Guibout C, Oberlin O, et al.: Role of cancer treatment in long-term overall and cardiovascular mortality after childhood cancer. J Clin Oncol 28 (8): 1308-15, 2010.
-
Kero AE, Järvelä LS, Arola M, et al.: Cardiovascular morbidity in long-term survivors of early-onset cancer: a population-based study. Int J Cancer 134 (3): 664-73, 2014.
-
Lipshultz SE, Adams MJ, Colan SD, et al.: Long-term cardiovascular toxicity in children, adolescents, and young adults who receive cancer therapy: pathophysiology, course, monitoring, management, prevention, and research directions: a scientific statement from the American Heart Association. Circulation 128 (17): 1927-95, 2013.
-
Armstrong GT, Oeffinger KC, Chen Y, et al.: Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol 31 (29): 3673-80, 2013.
-
Oeffinger KC, Mertens AC, Sklar CA, et al.: Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355 (15): 1572-82, 2006.
-
Hudson MM, Ness KK, Gurney JG, et al.: Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309 (22): 2371-81, 2013.
-
van Dalen EC, van der Pal HJ, Kok WE, et al.: Clinical heart failure in a cohort of children treated with anthracyclines: a long-term follow-up study. Eur J Cancer 42 (18): 3191-8, 2006.
-
Mulrooney DA, Yeazel MW, Kawashima T, et al.: Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 339: b4606, 2009.
-
van der Pal HJ, van Dalen EC, van Delden E, et al.: High risk of symptomatic cardiac events in childhood cancer survivors. J Clin Oncol 30 (13): 1429-37, 2012.
-
Haddy N, Diallo S, El-Fayech C, et al.: Cardiac Diseases Following Childhood Cancer Treatment: Cohort Study. Circulation 133 (1): 31-8, 2016.
-
Green DM, Grigoriev YA, Nan B, et al.: Congestive heart failure after treatment for Wilms' tumor: a report from the National Wilms' Tumor Study group. J Clin Oncol 19 (7): 1926-34, 2001.
-
Schellong G, Riepenhausen M, Bruch C, et al.: Late valvular and other cardiac diseases after different doses of mediastinal radiotherapy for Hodgkin disease in children and adolescents: report from the longitudinal GPOH follow-up project of the German-Austrian DAL-HD studies. Pediatr Blood Cancer 55 (6): 1145-52, 2010.
-
Green DM, Kun LE, Matthay KK, et al.: Relevance of historical therapeutic approaches to the contemporary treatment of pediatric solid tumors. Pediatr Blood Cancer 60 (7): 1083-94, 2013.
-
Hudson MM, Neglia JP, Woods WG, et al.: Lessons from the past: opportunities to improve childhood cancer survivor care through outcomes investigations of historical therapeutic approaches for pediatric hematological malignancies. Pediatr Blood Cancer 58 (3): 334-43, 2012.
-
Moslehi JJ: Cardiovascular Toxic Effects of Targeted Cancer Therapies. N Engl J Med 375 (15): 1457-1467, 2016.
-
Chow EJ, Chen Y, Kremer LC, et al.: Individual prediction of heart failure among childhood cancer survivors. J Clin Oncol 33 (5): 394-402, 2015.
-
Bhakta N, Liu Q, Yeo F, et al.: Cumulative burden of cardiovascular morbidity in paediatric, adolescent, and young adult survivors of Hodgkin's lymphoma: an analysis from the St Jude Lifetime Cohort Study. Lancet Oncol 17 (9): 1325-34, 2016.
-
Zhang S, Liu X, Bawa-Khalfe T, et al.: Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med 18 (11): 1639-42, 2012.
-
Silber JH, Cnaan A, Clark BJ, et al.: Enalapril to prevent cardiac function decline in long-term survivors of pediatric cancer exposed to anthracyclines. J Clin Oncol 22 (5): 820-8, 2004.
-
Lipshultz SE, Lipsitz SR, Sallan SE, et al.: Chronic progressive cardiac dysfunction years after doxorubicin therapy for childhood acute lymphoblastic leukemia. J Clin Oncol 23 (12): 2629-36, 2005.
-
Hudson MM, Rai SN, Nunez C, et al.: Noninvasive evaluation of late anthracycline cardiac toxicity in childhood cancer survivors. J Clin Oncol 25 (24): 3635-43, 2007.
-
van der Pal HJ, van Dalen EC, Hauptmann M, et al.: Cardiac function in 5-year survivors of childhood cancer: a long-term follow-up study. Arch Intern Med 170 (14): 1247-55, 2010.
-
Armenian SH, Hudson MM, Mulder RL, et al.: Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol 16 (3): e123-36, 2015.
-
Armenian SH, Sun CL, Vase T, et al.: Cardiovascular risk factors in hematopoietic cell transplantation survivors: role in development of subsequent cardiovascular disease. Blood 120 (23): 4505-12, 2012.
-
Children's Oncology Group: Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, Version 4.0. Monrovia, Ca: Children's Oncology Group, 2013. Available online. Last accessed April 14, 2017.
-
Le Deley MC, Leblanc T, Shamsaldin A, et al.: Risk of secondary leukemia after a solid tumor in childhood according to the dose of epipodophyllotoxins and anthracyclines: a case-control study by the Société Française d'Oncologie Pédiatrique. J Clin Oncol 21 (6): 1074-81, 2003.
-
Keefe DL: Anthracycline-induced cardiomyopathy. Semin Oncol 28 (4 Suppl 12): 2-7, 2001.
-
Feijen EA, Leisenring WM, Stratton KL, et al.: Equivalence Ratio for Daunorubicin to Doxorubicin in Relation to Late Heart Failure in Survivors of Childhood Cancer. J Clin Oncol 33 (32): 3774-80, 2015.
-
van Dalen EC, Michiels EM, Caron HN, et al.: Different anthracycline derivates for reducing cardiotoxicity in cancer patients. Cochrane Database Syst Rev (5): CD005006, 2010.
-
van Dalen EC, van der Pal HJ, Caron HN, et al.: Different dosage schedules for reducing cardiotoxicity in cancer patients receiving anthracycline chemotherapy. Cochrane Database Syst Rev (4): CD005008, 2009.
-
Lipshultz SE, Giantris AL, Lipsitz SR, et al.: Doxorubicin administration by continuous infusion is not cardioprotective: the Dana-Farber 91-01 Acute Lymphoblastic Leukemia protocol. J Clin Oncol 20 (6): 1677-82, 2002.
-
Hensley ML, Hagerty KL, Kewalramani T, et al.: American Society of Clinical Oncology 2008 clinical practice guideline update: use of chemotherapy and radiation therapy protectants. J Clin Oncol 27 (1): 127-45, 2009.
-
van Dalen EC, Caron HN, Dickinson HO, et al.: Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev (6): CD003917, 2011.
-
Wexler LH, Andrich MP, Venzon D, et al.: Randomized trial of the cardioprotective agent ICRF-187 in pediatric sarcoma patients treated with doxorubicin. J Clin Oncol 14 (2): 362-72, 1996.
-
Lipshultz SE, Scully RE, Lipsitz SR, et al.: Assessment of dexrazoxane as a cardioprotectant in doxorubicin-treated children with high-risk acute lymphoblastic leukaemia: long-term follow-up of a prospective, randomised, multicentre trial. Lancet Oncol 11 (10): 950-61, 2010.
-
Asselin BL, Devidas M, Chen L, et al.: Cardioprotection and Safety of Dexrazoxane in Patients Treated for Newly Diagnosed T-Cell Acute Lymphoblastic Leukemia or Advanced-Stage Lymphoblastic Non-Hodgkin Lymphoma: A Report of the Children's Oncology Group Randomized Trial Pediatric Oncology Group 9404. J Clin Oncol 34 (8): 854-62, 2016.
-
Shaikh F, Dupuis LL, Alexander S, et al.: Cardioprotection and Second Malignant Neoplasms Associated With Dexrazoxane in Children Receiving Anthracycline Chemotherapy: A Systematic Review and Meta-Analysis. J Natl Cancer Inst 108 (4): , 2016.
-
Schwartz CL, Constine LS, Villaluna D, et al.: A risk-adapted, response-based approach using ABVE-PC for children and adolescents with intermediate- and high-risk Hodgkin lymphoma: the results of P9425. Blood 114 (10): 2051-9, 2009.
-
Galper SL, Yu JB, Mauch PM, et al.: Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood 117 (2): 412-8, 2011.
-
Mulrooney DA, Nunnery SE, Armstrong GT, et al.: Coronary artery disease detected by coronary computed tomography angiography in adult survivors of childhood Hodgkin lymphoma. Cancer 120 (22): 3536-44, 2014.
-
Bowers DC, Liu Y, Leisenring W, et al.: Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol 24 (33): 5277-82, 2006.
-
De Bruin ML, Dorresteijn LD, van't Veer MB, et al.: Increased risk of stroke and transient ischemic attack in 5-year survivors of Hodgkin lymphoma. J Natl Cancer Inst 101 (13): 928-37, 2009.
-
Haddy N, Mousannif A, Tukenova M, et al.: Relationship between the brain radiation dose for the treatment of childhood cancer and the risk of long-term cerebrovascular mortality. Brain 134 (Pt 5): 1362-72, 2011.
-
Mueller S, Sear K, Hills NK, et al.: Risk of first and recurrent stroke in childhood cancer survivors treated with cranial and cervical radiation therapy. Int J Radiat Oncol Biol Phys 86 (4): 643-8, 2013.
-
Fullerton HJ, Stratton K, Mueller S, et al.: Recurrent stroke in childhood cancer survivors. Neurology 85 (12): 1056-64, 2015.
-
Mueller S, Fullerton HJ, Stratton K, et al.: Radiation, atherosclerotic risk factors, and stroke risk in survivors of pediatric cancer: a report from the Childhood Cancer Survivor Study. Int J Radiat Oncol Biol Phys 86 (4): 649-55, 2013.
-
Lipshultz SE, Landy DC, Lopez-Mitnik G, et al.: Cardiovascular status of childhood cancer survivors exposed and unexposed to cardiotoxic therapy. J Clin Oncol 30 (10): 1050-7, 2012.
-
Chao C, Xu L, Bhatia S, et al.: Cardiovascular Disease Risk Profiles in Survivors of Adolescent and Young Adult (AYA) Cancer: The Kaiser Permanente AYA Cancer Survivors Study. J Clin Oncol 34 (14): 1626-33, 2016.
-
Nandagopal R, Laverdière C, Mulrooney D, et al.: Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res 69 (2): 65-74, 2008.
-
Lipshultz SE, Lipsitz SR, Kutok JL, et al.: Impact of hemochromatosis gene mutations on cardiac status in doxorubicin-treated survivors of childhood high-risk leukemia. Cancer 119 (19): 3555-62, 2013.
-
Visscher H, Ross CJ, Rassekh SR, et al.: Validation of variants in SLC28A3 and UGT1A6 as genetic markers predictive of anthracycline-induced cardiotoxicity in children. Pediatr Blood Cancer 60 (8): 1375-81, 2013.
-
Wang X, Liu W, Sun CL, et al.: Hyaluronan synthase 3 variant and anthracycline-related cardiomyopathy: a report from the children's oncology group. J Clin Oncol 32 (7): 647-53, 2014.
-
Wang X, Sun CL, Quiñones-Lombraña A, et al.: CELF4 Variant and Anthracycline-Related Cardiomyopathy: A Children's Oncology Group Genome-Wide Association Study. J Clin Oncol 34 (8): 863-70, 2016.
-
Aminkeng F, Bhavsar AP, Visscher H, et al.: A coding variant in RARG confers susceptibility to anthracycline-induced cardiotoxicity in childhood cancer. Nat Genet 47 (9): 1079-84, 2015.
-
Visscher H, Rassekh SR, Sandor GS, et al.: Genetic variants in SLC22A17 and SLC22A7 are associated with anthracycline-induced cardiotoxicity in children. Pharmacogenomics 16 (10): 1065-76, 2015.
-
Davies SM: Getting to the heart of the matter. J Clin Oncol 30 (13): 1399-400, 2012.
-
Brouwer CA, Postma A, Hooimeijer HL, et al.: Endothelial damage in long-term survivors of childhood cancer. J Clin Oncol 31 (31): 3906-13, 2013.
-
Maraldo MV, Jørgensen M, Brodin NP, et al.: The impact of involved node, involved field and mantle field radiotherapy on estimated radiation doses and risk of late effects for pediatric patients with Hodgkin lymphoma. Pediatr Blood Cancer 61 (4): 717-22, 2014.
-
Landier W, Bhatia S, Eshelman DA, et al.: Development of risk-based guidelines for pediatric cancer survivors: the Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol 22 (24): 4979-90, 2004.
-
Skinner R, Wallace WH, Levitt GA, et al.: Long-term follow-up of people who have survived cancer during childhood. Lancet Oncol 7 (6): 489-98, 2006.
-
Shankar SM, Marina N, Hudson MM, et al.: Monitoring for cardiovascular disease in survivors of childhood cancer: report from the Cardiovascular Disease Task Force of the Children's Oncology Group. Pediatrics 121 (2): e387-96, 2008.
-
Morris B, Partap S, Yeom K, et al.: Cerebrovascular disease in childhood cancer survivors: A Children's Oncology Group Report. Neurology 73 (22): 1906-13, 2009.
-
Sieswerda E, Postma A, van Dalen EC, et al.: The Dutch Childhood Oncology Group guideline for follow-up of asymptomatic cardiac dysfunction in childhood cancer survivors. Ann Oncol 23 (8): 2191-8, 2012.
-
Armenian SH, Lacchetti C, Barac A, et al.: Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 35 (8): 893-911, 2017.
-
Lenihan DJ, Oliva S, Chow EJ, et al.: Cardiac toxicity in cancer survivors. Cancer 119 (Suppl 11): 2131-42, 2013.
-
Armstrong GT, Kawashima T, Leisenring W, et al.: Aging and risk of severe, disabling, life-threatening, and fatal events in the childhood cancer survivor study. J Clin Oncol 32 (12): 1218-27, 2014.
-
Chen AB, Punglia RS, Kuntz KM, et al.: Cost effectiveness and screening interval of lipid screening in Hodgkin's lymphoma survivors. J Clin Oncol 27 (32): 5383-9, 2009.
-
Wong FL, Bhatia S, Landier W, et al.: Cost-effectiveness of the children's oncology group long-term follow-up screening guidelines for childhood cancer survivors at risk for treatment-related heart failure. Ann Intern Med 160 (10): 672-83, 2014.
-
Yeh JM, Nohria A, Diller L: Routine echocardiography screening for asymptomatic left ventricular dysfunction in childhood cancer survivors: a model-based estimation of the clinical and economic effects. Ann Intern Med 160 (10): 661-71, 2014.
-
Landier W, Armenian SH, Lee J, et al.: Yield of screening for long-term complications using the children's oncology group long-term follow-up guidelines. J Clin Oncol 30 (35): 4401-8, 2012.
-
Ramjaun A, AlDuhaiby E, Ahmed S, et al.: Echocardiographic Detection of Cardiac Dysfunction in Childhood Cancer Survivors: How Long Is Screening Required? Pediatr Blood Cancer 62 (12): 2197-203, 2015.
-
Spewak MB, Williamson RS, Mertens AC, et al.: Yield of screening echocardiograms during pediatric follow-up in survivors treated with anthracyclines and cardiotoxic radiation. Pediatr Blood Cancer 64 (6): , 2017.
-
Jones LW, Liu Q, Armstrong GT, et al.: Exercise and risk of major cardiovascular events in adult survivors of childhood hodgkin lymphoma: a report from the childhood cancer survivor study. J Clin Oncol 32 (32): 3643-50, 2014.
Late Effects of the Central Nervous SystemNeurocognitive Neurocognitive late effects are most commonly observed after treatment of malignancies that require central nervous system (CNS)-directed therapies. While there is considerable evidence published about this outcome, its quality is often limited by small sample size, cohort selection and participation bias, cross-sectional versus prospective evaluations, and variable time of assessment from treatment exposures. CNS-directed therapies include the following: - Cranial radiation therapy.
- Systemic therapy with high-dose methotrexate or cytarabine.
- Intrathecal chemotherapy.
Children with brain tumors or acute lymphoblastic leukemia (ALL) are most likely to be affected. Risk factors for the development of neurocognitive late effects include the following:[1,2,3,4,5,6,7] - Female gender.
- Younger age at the time of treatment.
- Tumor location.
- Higher cranial radiation dose.
- Treatment with both cranial radiation therapy and chemotherapy (systemic or intrathecal).
- Lower socioeconomic status.
It should be noted that the cognitive phenotypes observed in childhood survivors of ALL and CNS tumors may differ from traditional developmental disorders. For example, the phenotype of attention problems in ALL and brain tumor survivors appears to differ from developmental attention-deficit/hyperactivity disorder in that few survivors demonstrate significant hyperactivity/impulsivity, but instead have associated difficulties with processing speed and executive function.[8,9] Neuroimaging studies of irradiated and nonirradiated ALL survivors demonstrate a variety of CNS abnormalities, including leukoencephalopathy, cerebral lacunes, cerebral atrophy, and dystrophic calcifications (mineralizing microangiopathy). Among these, abnormalities of cerebral white matter integrity and volume have been correlated with neurocognitive outcomes.[10,11,12,13] Cavernomas have also been observed in ALL survivors treated with cranial irradiation. They have been speculated to result from angiogenic processes as opposed to tumorigenesis.[14] Neurocognitive outcomes in brain tumor survivors Survival rates have increased over recent decades for children with brain tumors; however, long-term cognitive effects caused by illness and associated treatments are a well-established morbidity in this group of survivors. In childhood and adolescent brain tumor survivors, risk factors for adverse neurocognitive effects include the following: - Cranial radiation therapy. Cranial radiation therapy has been associated with the highest risk of long-term cognitive morbidity, particularly in younger children.[15] There is an established dose-response relationship, with patients who receive higher-dose cranial radiation therapy consistently performing more poorly on intellectual measures.[16] Radiation dose to specific subvolumes of the brain, including the temporal lobes and hippocampi, have been shown to significantly impact longitudinal intelligence quotient (IQ) scores and academic achievement scores among children treated with craniospinal irradiation for medulloblastoma.[17]
- Tumor site.[15]
- Shunted hydrocephalus.[15,18,19]
- Postsurgical cerebellar mutism.[20]
- Auditory difficulties, including sensorineural hearing loss.[18,21]
- History of stroke.[22]
The negative impact of radiation treatment has been characterized by changes in IQ scores, which have been noted to drop about 2 to 5 years after diagnosis; the decline continues 5 to 10 years afterward, although less is known about potential stabilization or further decline of IQ scores several decades after diagnosis.[23,24,25] The decline in IQ scores over time typically reflects the child's failure to acquire new abilities or information at a rate similar to that of his or her peers, rather than a progressive loss of skills and knowledge.[16] Affected children also may experience deficits in other cognitive areas, including academic difficulties (reading and math) and problems with attention, processing speed, memory, and visual or perceptual motor skills.[24,26,27] These changes in cognitive functioning may be partially explained by radiation-induced reduction of normal-appearing white matter volume or integrity of white matter pathways, as evaluated through magnetic resonance imaging (MRI).[28,29,30] In fact, reduced white matter integrity has been directly linked to slowed cognitive processing speed in survivors of brain tumors,[31] while greater white matter volume has been associated with better working memory, particularly in females.[30] It should be noted that data emerging from contemporary protocols show that using lower doses of cranial radiation and more targeted treatment volumes appears to reduce the severity of neurocognitive effects of therapy.[19,32] Data are emerging regarding cognitive outcomes after proton radiation to the CNS.[33,34] To date, these studies largely describe IQ changes during early (less than 5 years from radiation) follow-up and are limited by retrospective analysis of cognitive outcomes among relatively small clinically heterogeneous pediatric brain tumor cohorts and use of historically treated photon patients or population standards as comparison groups. Study results demonstrating lack of difference in slopes of IQ change among photon- and proton-treated patients [33] and significant declines in cognitive processing speed among patients treated with proton radiation [34] underscore the importance of longitudinal follow-up to determine whether proton radiation provides a clinically meaningful benefit in sparing cognitive function compared with photon radiation. Longitudinal follow-up is critical to confirm the superiority of proton versus photon therapy in preserving cognitive function. Longitudinal cohort studies have provided insight into the trajectory and predictors of cognitive decline among survivors of CNS tumors. Results of representative cohort studies include the following: - A report from St. Jude Children's Research Hospital showed cognitive decline after 54 Gy of conformal cranial radiation therapy in 78 children younger than 20 years (mean, 9.7 years) diagnosed with low-grade glioma (refer to Figure 5). Age at time of cranial irradiation was more important than was cranial radiation dose in predicting cognitive decline, with children younger than 5 years estimated to experience the greatest cognitive decline.[35]
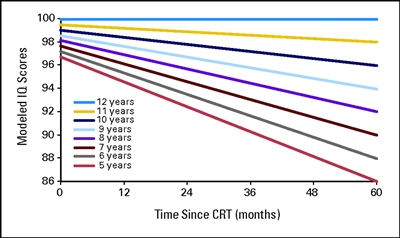
Figure 5. Modeled intelligence quotient (IQ) scores after conformal radiation therapy (CRT) by age for pediatric low-grade glioma. Age is measured in years, and time is measured in months after the start of CRT. Thomas E. Merchant, Heather M. Conklin, Shengjie Wu, Robert H. Lustig, and Xiaoping Xiong, Late Effects of Conformal Radiation Therapy for Pediatric Patients With Low-Grade Glioma: Prospective Evaluation of Cognitive, Endocrine, and Hearing Deficits, Journal of Clinical Oncology, volume 27, issue 22, pages 3691-3697. Reprinted with permission. © (2009) American Society of Clinical Oncology. All rights reserved.
- In a study of 126 medulloblastoma survivors treated with 23.4 Gy or 36 Gy to 39.6 Gy of cranial spinal radiation (with a conformal boost dose of 55.8 Gy to the primary tumor bed), processing speed scores declined significantly over time, while less decline was observed in attention and memory performance. Higher doses of radiation and younger age at diagnosis predicted slower processing speed over time.[36] Studies of working memory and academic achievement in patients enrolled on the same medulloblastoma trial (St. Jude SJMB03 [NCT00085202]) indicated that performance was largely within the age-expected range up to 5 years postdiagnosis,[37,38] although in both studies, posterior fossa syndrome, higher cranial radiation dose, and younger age at diagnosis predicted worse performance over time. In addition, serious hearing loss was associated with intellectual and academic decline over time.[38]
- Canadian investigators evaluated the impact of radiation (dose and boost volume) and neurologic complications on patterns of intellectual functioning in a cohort of 113 medulloblastoma survivors (mean age at diagnosis, 7.5 years; mean time from diagnosis to last assessment, 6 years). Survivors treated with reduced-dose craniospinal radiation therapy plus tumor bed boost showed stable intellectual functioning. Neurological complications, such as hydrocephalus requiring cerebrospinal fluid diversion and mutism, and treatment with higher doses and larger boost volumes of radiation resulted in intellectual declines with distinctive trajectories.[39]
Although adverse neurocognitive outcomes observed 5 to 10 years after treatment are presumed to be pervasive, and potentially worsen over time, few empirical data are available regarding the neurocognitive functioning in very long-term survivors of CNS tumors. - Among adult survivors participating in the Childhood Cancer Survivor Study (CCSS), CNS tumor survivors (n = 802) reported significantly more problems with attention/processing speed, memory, emotional control, and organization than did survivors of non-CNS malignancies (n = 5,937) and sibling controls (n = 382).[4] Moreover, a large proportion of CNS tumor survivors treated with cranial irradiation reported impairment on measures of attention/processing speed (42.9%-73.3%) and memory (14.3%-37.4%), with differences observed by diagnosis and cranial radiation dose.[40]
The neurocognitive consequences of CNS disease and treatment may have a considerable impact on functional outcomes for brain tumor survivors. - In childhood and adolescence, neurocognitive deficits have been associated with poor social adjustment, including problems with peer relations, social withdrawal, and reduced social skills.[41,42]
- CNS tumor survivors are more likely to need special education services than are survivors of other malignancies.[43]
- Adult CNS tumor survivors are less likely to live independently, marry, and graduate from college than are survivors of other malignancies and siblings.[43,44,45]
Neurocognitive outcomes in acute lymphoblastic leukemia (ALL) survivors The increase in cure rates for children with ALL over the past decades has resulted in greater attention to the neurocognitive morbidity and quality of life of survivors. The goal of current ALL treatment is to minimize adverse late effects while maintaining high survival rates. To minimize the risk of late sequelae, patients are stratified for treatment according to their risk of relapse. Cranial irradiation is reserved for the fewer than 20% of children who are considered at high risk for CNS relapse.[46] Although low-risk, standard-risk, and most high-risk patients are treated with chemotherapy-only protocols, early reports of neurocognitive late effects for ALL patients were based on heterogeneously treated groups of survivors who were treated with combinations (simultaneously or sequentially) of intrathecal chemotherapy, radiation therapy, and high-dose chemotherapy, making it difficult to differentiate the impact of the individual treatment components. However, outcome data are increasingly available regarding the risk of neurocognitive late effects in survivors of childhood ALL treated with chemotherapy only. ALL and cranial radiation In survivors of ALL, cranial radiation therapy may result in clinical and radiographic neurologic late sequelae. Clinical leukoencephalopathy characterized by spasticity, ataxia, dysarthria, dysphagia, hemiparesis, and seizures is uncommon after contemporary ALL therapy. In contrast, neuroimaging frequently demonstrates white matter abnormalities among survivors treated with cranial irradiation and/or high-dose methotrexate. Radiographic leukoencephalopathy has been reported in up to 80% of children on some treatment regimens. Higher doses and more courses of intravenous methotrexate have been reported to increase risk of leukoencephalopathy.[10] In many patients, white matter anomalies are transient and decrease in prevalence, extent, and intensity with longer elapsed time from completion of therapy.[10] Leukoencephalopathy results in smaller white matter volumes that have been correlated with cognitive deficits. Although these abnormalities are mild among the irradiated patients (overall IQ fall of approximately 10 points), those who have received higher doses at a young age may have significant learning difficulties.[47,48] Deficits in neuropsychological functions such as visual-motor integration, processing speed, attention, and short-term memory are reported in children treated with 18 Gy to 24 Gy.[47,49,50] Girls and children treated at a younger age are more vulnerable to cranial radiation.[51] The decline in intellectual functioning appears to be progressive, showing more impairment of cognitive function with increasing time since radiation therapy.[51,52] Limited studies suggest that long-term survivors of childhood ALL treated with cranial irradiation are at risk of progressive decline consistent with early-onset mild cognitive impairment; this risk is most prominent among those treated with cranial radiation doses of 24 Gy.[12,53] ALL and chemotherapy-only CNS therapy Because of its penetrance into the CNS, systemic methotrexate has been used in a variety of low-dose and high-dose regimens for leukemia CNS prophylaxis. Systemic methotrexate in high doses with or without radiation therapy can lead to an infrequent but well-described leukoencephalopathy, which has been linked to neurocognitive impairment.[10] When neurocognitive outcomes after radiation therapy and chemotherapy-only regimens are directly compared, the evidence suggests a better outcome for those treated with chemotherapy alone, although some studies show no significant difference.[54,55] Compared with cranial irradiation, chemotherapy-only CNS-directed treatment produces neurocognitive deficits involving processes of attention, speed of information processing, memory, verbal comprehension, visual-spatial skills, visual-motor functioning, and executive functioning; global intellectual function is typically preserved.[49,54,56,57,58,59] Few longitudinal studies evaluating long-term neurocognitive outcome report adequate data for a decline in global IQ after treatment with chemotherapy alone.[57] The academic achievement of ALL survivors in the long term seems to be generally average for reading and spelling, with deficits mainly affecting arithmetic performance.[54,60,61] Risk factors for poor neurocognitive outcome after chemotherapy-only CNS-directed treatment are younger age and female gender.[59,62,63] Reduced cognitive status has been observed in association with reduced integrity in neuroanatomical regions essential in memory formation (e.g., reduced hippocampal volume with increased activation and thinner parietal cortices). However, the long-term impact of these prevalent neurocognitive and neuroimaging abnormalities on functional status in aging adults treated for childhood ALL, particularly those treated with contemporary chemotherapy alone approaches, remains an active area of research. Studies of neurocognitive functioning in large pediatric cancer survivor cohorts observed the following: - In the St. Jude Total XV (NCT00137111) trial, which omitted prophylactic cranial irradiation, comprehensive cognitive testing of 243 participants at week 120 revealed higher risk for below-average performance on a measure of sustained attention but not on measures of intellectual functioning, academic skills, or memory. The risk of cognitive deficits correlated with treatment intensity but not with age at diagnosis or gender. Prolonged follow-up (average, 7.7 years from diagnosis) of this cohort demonstrated that intelligence was within normal limits compared with population expectations, but measures of executive function, processing speed, and memory were less than population means. Higher plasma methotrexate was associated with executive dysfunction, thicker cerebral cortex, and higher activity in frontal brain regions on functional MRI.[64] These results underscore the need for continued follow-up as this population ages to better characterize the prevalence and magnitude of cognitive deficits after CNS-directed therapy with chemotherapy alone.[65]
- In a large prospective study (N = 555) of neurocognitive outcomes in children with newly diagnosed ALL who were randomly assigned to receive CNS-directed therapy according to risk group (low risk: intrathecal methotrexate vs. high-dose methotrexate; high risk: high-dose methotrexate vs. 24 Gy cranial radiation therapy), a significant reduction in IQ scores (4-7 points) was observed in all patient groups when compared with controls, regardless of the CNS treatment delivered. Children younger than 5 years at diagnosis were more likely to have IQs below 80 at 3 years posttherapy than were children older than 5 years at diagnosis, irrespective of treatment allocation, suggesting that younger children are more vulnerable to treatment-related neurologic toxic effects.[66]
- Persistent cognitive deficits and progressive intellectual decline have been observed in cohorts of adults treated for ALL during childhood and associated with reduced educational attainment and unemployment.[12,48,51] According to the results of neurocognitive testing and patient reported outcomes in more than 500 adult survivors of childhood ALL at 26 years postdiagnosis, survivors demonstrated increased rates of impairment in most neurocognitive and behavioral domains. Impairment was common in survivors treated with lower doses of cranial radiation and in those treated with chemotherapy only. Impairment in executive function skills increased with time since diagnosis; impairment in intellect, academics, and memory progressively increased with younger age at treatment in a cranial radiation dose-dependent manner; and neurocognitive function was related to functional outcomes as adults, including college graduation and full-time employment. Continued monitoring by health professionals is recommended to identify neurocognitive problems that may emerge over time.[48]
ALL and steroid therapy The type of steroid used for ALL systemic treatment may affect cognitive functioning. In a study that involved long-term neurocognitive testing (mean follow-up, 9.8 years) in 92 children with a history of standard-risk ALL who had received either dexamethasone or prednisone during treatment, no meaningful differences in mean neurocognitive and academic performance scores were observed.[67] In contrast, in a study of 567 adult survivors of childhood leukemia (mean age, 33 years; mean time since diagnosis, 26 years) dexamethasone exposure was associated with increased risk of impairment in attention (relative risk [RR], 2.12; 95% confidence interval [CI], 1.11-4.03) and executive function (RR, 2.42; 95% CI, 1.20-4.91), independent of methotrexate exposure. Intrathecal hydrocortisone also increased risk of attention problems (RR, 1.24; 95% CI, 1.05-1.46).[48] Other cancers Neurocognitive abnormalities have been reported in other groups of cancer survivors. In a study of adult survivors of childhood non-CNS cancers (including ALL, n = 5,937), 13% to 21% of survivors reported impairment in task efficiency, organization, memory, or emotional regulation. This rate of impairment was approximately 50% higher than that reported in the sibling comparison group. Factors such as diagnosis before age 6 years, female gender, cranial radiation therapy, and hearing impediment were associated with impairment.[50] In a study evaluating neurocognitive function among 80 long-term survivors of osteosarcoma (mean time since diagnosis, 24.7 years), survivors demonstrated lower mean scores in reading skills, attention, memory, and processing speed than did community controls. Neurocognitive outcomes showed significant associations with current chronic health conditions impacting cardiac, pulmonary, and endocrine function.[68] Stem cell transplantation Cognitive and academic consequences of stem cell transplantation in children have also been evaluated and include the following: - In a report from St. Jude Children's Research Hospital in which 268 patients were treated with stem cell transplantation, minimal risk of late cognitive and academic sequelae was observed. Subgroups of patients were at relatively higher risk, including patients who underwent unrelated donor transplantation, received total-body irradiation, and developed graft-versus-host disease (GVHD). However, these differences were small relative to differences in premorbid functioning, particularly those associated with socioeconomic status.[69]
- In a series of 38 patients who underwent hematopoietic stem cell transplantation (HSCT) and received intrathecal chemotherapy, significant declines in visual motor skills and memory scores were noted within the first year posttransplant. By 3 years posttransplant, there was an improvement in visual motor development scores and memory scores, but new deficits were evident in long-term memory scores. By 5 years posttransplant, there were progressive declines in verbal skills and performance skills, and new deficits were seen in long-term verbal memory scores. The greatest decline in neurocognitive function occurred in patients who received cranial irradiation, either as part of their initial therapy or as part of their HSCT conditioning.[70]
Most neurocognitive late effects after stem cell transplantation are thought to be related to white matter damage in the brain. This was investigated in children with leukemia who were treated with HSCT. In a series of 36 patients, performance on neurocognitive measures typically associated with white matter was compared with performance on measures thought to correlate with gray matter function. Composite white matter scores were significantly lower than composite gray matter scores, thereby supporting the belief that white matter damage contributes to neurocognitive late effects in this population.[71] Neurologic Sequelae Risk of neurologic complications may be predisposed by the following: - Tumor location.
- Neurosurgery.
- Cranial radiation therapy.
- Specific neurotoxic chemotherapeutic agents.
In children with CNS tumors, mass effect, tumor infiltration, and increased intracranial pressure may result in motor or sensory deficits, cerebellar dysfunction, and secondary effects such as seizures and cerebrovascular complications. Numerous reports describe abnormalities of CNS integrity and function, but such studies are typically limited by small sample size, cohort selection and participation bias, cross-sectional ascertainment of outcomes, and variable time of assessment from treatment exposures. In contrast, relatively few studies comprehensively or systematically ascertain outcomes related to peripheral nervous system function. Neurologic complications that may occur in adult survivors of childhood cancer include the following: - Leukoencephalopathy. Clinical or radiographic leukoencephalopathy has been reported after cranial irradiation and high-dose systemic methotrexate administration. Younger patients and those treated with cranial radiation doses higher than 24 Gy are more vulnerable to reduced white matter volumes associated with leukoencephalopathy.[11,12,13,49] White matter changes may be accompanied by other neuroimaging abnormalities, including dystrophic calcifications, cerebral lacunae, and cerebral atrophy.
- Peripheral neuropathy. Vinca alkaloid agents (vincristine and vinblastine) and cisplatin may cause peripheral neuropathy. This condition presents during treatment and appears to improve or clinically resolve after completion of therapy.[72] However, higher cumulative doses of vincristine and/or intrathecal methotrexate have been linked to neuromuscular impairments in long-term survivors of childhood ALL, which suggests that persistent effects of these agents may affect functional status in aging survivors.[73]
Among adult survivors of extracranial solid tumors of childhood (median time from diagnosis, 25 years), standardized assessment of neuromuscular function disclosed motor impairment in association with vincristine exposure and sensory impairment in association with cisplatin exposure.[74] Survivors with sensory impairment demonstrated a higher prevalence of functional performance limitations related to poor endurance and mobility restrictions. These studies underscore the importance of assessment and referral to rehabilitative services to optimize functional outcomes among long-term survivors. - Stroke. Refer to the cerebrovascular disease section of this summary for information on stroke.
- Other neurologic sequelae. In a report from the CCSS that compared self-reported neurologic late effects among 4,151 adult survivors of childhood ALL with siblings, survivors were at elevated risk for late-onset coordination problems, motor problems, seizures, and headaches. The overall cumulative incidence was 44% at 20 years. Serious headaches were most common, with a cumulative incidence of 25.8% at 20 years, followed by focal neurologic dysfunction (21.2%) and seizures (7%). Children who were treated with regimens that included cranial irradiation for ALL and those who suffered relapse were at increased risk for late-onset neurologic sequelae.[75]
In a cross-sectional study that evaluated neurologic morbidity and quality of life in 162 survivors of childhood ALL (median age at evaluation, 15.7 years; median time from completion of therapy, 7.4 years) in concert with a clinical neurologic exam, neurologic symptoms were present in 83% of survivors, but symptom-related morbidity was low and quality of life was high in most survivors. The most commonly reported symptoms included neuropathy (63%), headache (46.9%), dizziness (33.3%), and back pain (22.8%). Female gender, ten doses or more of intrathecal chemotherapy, and history of relapse were significant predictors for impaired quality of life.[7] Table 3. Central Nervous System Late Effectsa| Predisposing Therapy | Neurologic Effects | Health Screening |
|---|
| IQ = intelligence quotient; IT = intrathecal; IV = intravenous. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Platinum agents (carboplatin, cisplatin) | Peripheral sensory neuropathy | Neurologic exam | | Plant alkaloid agents (vinblastine, vincristine) | Peripheral sensory or motor neuropathy (areflexia, weakness, foot drop, paresthesias) | Neurologic exam | | Methotrexate (high dose IV or IT); cytarabine (high dose IV or IT); radiation impacting the brain | Clinical leukoencephalopathy (spasticity, ataxia, dysarthria, dysphagia, hemiparesis, seizures); headaches; seizures; sensory deficits | History: cognitive, motor, and/or sensory deficits, seizures | | Neurologic exam | | Radiation impacting cerebrovascular structures | Cerebrovascular complications (stroke, moyamoya, occlusive cerebral vasculopathy) | History: transient/permanent neurological events | | Blood pressure | | Neurologic exam | | Neurosurgery-brain | Motor and/or sensory deficits (paralysis, movement disorders, ataxia, eye problems [ocular nerve palsy, gaze paresis, nystagmus, papilledema, optic atrophy]); seizures | Neurologic exam | | Neurology evaluation | | Neurosurgery-brain | Hydrocephalus; shunt malfunction | Abdominal x-ray | | Neurosurgery evaluation | | Neurosurgery-spine | Neurogenic bladder; urinary incontinence | History: hematuria, urinary urgency/frequency, urinary incontinence/retention, dysuria, nocturia, abnormal urinary stream | | Neurosurgery-spine | Neurogenic bowel; fecal incontinence | History: chronic constipation, fecal soiling | | Rectal exam | | Predisposing Therapy | Neuropsychological Effects | Health Screening | | Methotrexate (high-dose IV or IT); cytarabine (high-dose IV or IT); radiation impacting the brain; neurosurgery-brain | Neurocognitive deficits (executive function, memory, attention, processing speed, etc.); learning deficits; diminished IQ; behavioral change | Assessment of educational and vocational progress | | Formal neuropsychological evaluation | Psychosocial Many childhood cancer survivors report reduced quality of life or other adverse psychosocial outcomes. Evidence for adverse psychosocial adjustment after childhood cancer has been derived from a spectrum of sources, ranging from patient-reported or proxy-reported outcomes to data from population-based registries. The former may be limited by small sample size, cohort selection and participation bias, and variable methods and venues (clinical vs. distance-based survey) of assessments. The latter is often not well correlated with clinical and treatment characteristics that permit the identification of survivors at high risk of psychosocial deficits. Survivors with neurocognitive deficits are particularly vulnerable to adverse psychosocial outcomes that affect achievement of expected social competence during adulthood. - In a population-based study of adult survivors of CNS tumors diagnosed in childhood or adolescence, survivors had significantly poorer self-perception and self-esteem outcomes than did those of the general population. Female gender, persistent visible physical sequelae, specific tumor type, and treatment with cranial radiation therapy predicted self-perception outcomes.[76]
- In a series of CNS malignancy survivors (n = 802) reported from the CCSS, adverse outcome in indicators of successful adult adaptation (educational attainment, income, employment, and marital status) were most likely in survivors who report neurocognitive dysfunction.[4]
- Collectively, studies evaluating psychosocial outcomes among CNS tumor survivors indicate deficits in social competence that worsen over time.[77]
- In a CCSS study that evaluated predictors of independent living status across diagnostic groups, adult survivors of childhood cancer with neurocognitive, psychological, or physical late effects were less likely to live independently as adults than were siblings in the control group.[44]
- In a St. Jude Lifetime Cohort study of 224 survivors of CNS tumors (median current age, 26 years; median time from diagnosis, 18 years), neurocognitive impairment was significantly associated with lower educational attainment, unemployment, and nonindependent living.[78]
Childhood cancer survivors are also at risk of developing symptoms of psychological distress. In a longitudinal study of more than 4,500 survivors, subgroups of survivors were found to be at risk of developing persistent and increasing symptoms of anxiety and depression during a 16-year period. Survivors who reported pain and worsening health status were at the greatest risk of developing symptoms of anxiety, depression, and somatization over time.[79] Adult survivors of childhood cancer are also at risk of suicide ideation compared with siblings, with survivors of CNS tumors being most likely to report thoughts of suicide. In a CCSS study that evaluated the prevalence of recurrent suicidal ideation among 9,128 adult long-term survivors of childhood cancer, survivors were more likely to report late suicidal ideation (odds ratio [OR], 51.9; 95% CI, 51.5-2.5) and recurrent suicidal ideation (OR, 52.6; 95% CI, 51.8-3.8) compared with siblings.[80] History of seizure was associated with a twofold increased likelihood of suicide ideation in survivors. The presence of chronic health conditions can also impact aspects of psychological health. In a study that evaluated psychological outcomes among long-term survivors treated with HSCT, 22% of survivors and 8% of sibling controls reported adverse outcomes. Somatic distress was the most prevalent condition and affected 15% of HSCT survivors, representing a threefold higher risk compared with siblings. HSCT survivors with severe or life-threatening health conditions and active chronic GVHD had a twofold increased risk of somatic distress.[81] Incorporation of psychological screening into clinical visits for childhood cancer survivors may be valuable; however, limiting such evaluations to those returning to long-term follow-up clinics may result in a biased subsample of survivors with more difficulties, and precise prevalence rates may be difficult to establish. A review of behavioral, emotional, and social adjustment among survivors of childhood brain tumors illustrates this point, with the prevalence of psychological maladjustment ranging from 25% to 93%.[82] In a study of 101 adult cancer survivors of childhood cancer, psychological screening was performed during a routine annual evaluation at the survivorship clinic at the Dana Farber Cancer Institute. On the Symptom Checklist 90 Revised, 32 subjects had a positive screen (indicating psychological distress), and 14 subjects reported at least one suicidal symptom. Risk factors for psychological distress included subjects' dissatisfaction with physical appearance, poor physical health, and treatment with cranial irradiation. In this study, the instrument was shown to be feasible for use in the clinic visit setting because the psychological screening was completed in less than 30 minutes. In addition, completion of the instrument itself did not appear to cause distress in the survivors in 80% of cases.[83] These data support the feasibility and importance of consistent assessment of psychosocial distress in a medical clinic setting. (Refer to the PDQ summary on Adjustment to Cancer: Anxiety and Distress for more information about psychological distress and cancer patients.) Post-traumatic stress after childhood cancer Despite the many stresses associated with the diagnosis of cancer and its treatment, studies have generally shown low levels of post-traumatic stress symptoms and post-traumatic stress disorder (PTSD) in children with cancer, typically no higher than those in healthy comparison children.[84] Patient and parent adaptive style are significant determinants of PTSD in the pediatric oncology setting.[85,86] The prevalence of PTSD and post-traumatic stress symptoms has been reported in 15% to 20% of young adult survivors of childhood cancer, with estimates varying based on criteria used to define these conditions.[87] - Survivors with PTSD reported more psychological problems and negative beliefs about their illness and health status than did those without PTSD.[88,89]
- A subset of adult survivors (9%) from the CCSS reported functional impairment and/or clinical distress in addition to the set of symptoms consistent with a full diagnosis of PTSD. This was significantly more prevalent in survivors than in sibling comparisons.[90] In this study, PTSD was significantly associated with being unmarried, having an annual income of less than $20,000, being unemployed, having a high school education or less, and being older than 30 years. Survivors who were treated with cranial irradiation before age 4 years were at particularly high risk for PTSD. Intensive treatment was also associated with increased risk of full PTSD.
Because avoidance of places and persons associated with the cancer is part of PTSD, the syndrome may interfere with obtaining appropriate health care. Those with PTSD perceive greater current threats to their lives or the lives of their children. Other risk factors include poor family functioning, decreased social support, and noncancer stressors.[91] Psychosocial outcomes among childhood, adolescent, and young adult cancer survivors Most research on late effects after cancer has focused on individuals with a cancer manifestation during childhood. Little is known about the specific impact of a cancer diagnosis with an onset in adolescence or the impact of childhood cancer on adolescent and young adult psychosocial outcomes. The following studies describe psychosocial outcomes among these groups: - In 820 adult survivors of cancer diagnosed during adolescence (between ages 15 and 18 years), when compared with an age-matched sample from the general population and a control group of adults without cancer, female survivors of adolescent cancers achieved fewer developmental milestones in their psychosexual development, such as having their first boyfriend, or reached these milestones later. Male survivors were more likely to live with their parents than were same-sex controls. Adolescent cancer survivors were less likely to have ever married or have had children. Survivors were significantly older at their first marriage and at the birth of their first child than were their age-matched samples.[92]
Survivors in this cohort were also significantly less satisfied with their general and health-related life than were people in a community-based control group. Impaired general and health-related life satisfaction were associated with somatic late effects, symptoms of depression and anxiety, and lower rates of posttraumatic growth.[93] - In a survey of 4,054 adolescent and young adult (AYA) cancer survivors and 345,592 respondents who had no history of cancer, AYA cancer survivors were more likely to smoke (26% vs. 18%), be obese (31% vs. 27%), and have chronic conditions such as cardiovascular disease (14% vs. 7%), hypertension (35% vs. 9%), asthma (15% vs. 8%), disability (36% vs. 18%), and poor mental health (20% vs. 10%). They were also less likely to receive medical care because of cost (24% vs. 15%).[94]
- The CCSS evaluated outcomes of 2,979 adolescent survivors and 649 siblings of cancer survivors to determine the incidence of difficulty in six behavioral and social domains (depression/anxiety, being headstrong, attention deficit, peer conflict/social withdrawal, antisocial behaviors, and social competence).[95] Survivors were 1.5 times (99% CI, 1.1-2.1) more likely than were siblings to have symptoms of depression/anxiety and 1.7 times (99% CI, 1.3-2.2) more likely than were siblings to have antisocial behaviors. Scores in the depression/anxiety, attention deficit, and antisocial domains were significantly elevated in adolescents treated for leukemia or CNS tumors, compared with the scores in siblings. In addition, survivors of neuroblastoma had difficulty in the depression/anxiety and antisocial domains. CNS-directed treatments (cranial radiation therapy and/or intrathecal methotrexate) were specific risk factors for adverse behavioral outcomes.
- Another CCSS study evaluated psychological and neurocognitive function in 2,589 long-term cancer survivors who were diagnosed during adolescence and young adulthood.[96] Compared with a sibling cohort, survivors diagnosed during adolescence and young adulthood reported higher rates of depression (OR, 1.55; 95% CI, 1.04-2.30) and anxiety (OR, 2.00; 95% CI, 1.17-3.43) and reported more cognitive problems affecting task efficiency (OR, 1.72; 95% CI, 1.21-2.43), emotional regulation (OR, 1.74; 95% CI, 1.26-2.40), and memory (OR, 1.44; 95% CI, 1.09-1.89). Survivors of lymphoma and sarcoma diagnosed during later adolescence were at reduced risk of psychosocial and neurocognitive problems than were those diagnosed before age 11 years. These outcomes did not differ by age at diagnosis among CNS tumor and leukemia survivors. Survivors diagnosed during adolescence and young adulthood were also significantly less likely than sibling controls to have attained a post-high school education, be working full time, be married, or be living independently; inferior social outcomes were related to neurocognitive symptoms.
It should be noted that social withdrawal in adolescence was associated with adult obesity and physical inactivity.[97] As a result, these psychological problems may increase future risk for chronic health conditions and support the need to routinely screen and treat psychological problems after cancer therapy. Because of the challenges experienced by adolescents and young adults at cancer diagnosis and during long-term follow-up, this group needs to have access to programs to address the unique psychosocial, educational, and vocational issues that impact their transition to survivorship.[98,99] Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for CNS and psychosocial late effects information, including risk factors, evaluation, and health counseling. References:
-
Nathan PC, Patel SK, Dilley K, et al.: Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children's Oncology Group. Arch Pediatr Adolesc Med 161 (8): 798-806, 2007.
-
Robinson KE, Kuttesch JF, Champion JE, et al.: A quantitative meta-analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatr Blood Cancer 55 (3): 525-31, 2010.
-
Reeves CB, Palmer SL, Reddick WE, et al.: Attention and memory functioning among pediatric patients with medulloblastoma. J Pediatr Psychol 31 (3): 272-80, 2006.
-
Ellenberg L, Liu Q, Gioia G, et al.: Neurocognitive status in long-term survivors of childhood CNS malignancies: a report from the Childhood Cancer Survivor Study. Neuropsychology 23 (6): 705-17, 2009.
-
Butler RW, Fairclough DL, Katz ER, et al.: Intellectual functioning and multi-dimensional attentional processes in long-term survivors of a central nervous system related pediatric malignancy. Life Sci 93 (17): 611-6, 2013.
-
Patel SK, Mullins WA, O'Neil SH, et al.: Neuropsychological differences between survivors of supratentorial and infratentorial brain tumours. J Intellect Disabil Res 55 (1): 30-40, 2011.
-
Khan RB, Hudson MM, Ledet DS, et al.: Neurologic morbidity and quality of life in survivors of childhood acute lymphoblastic leukemia: a prospective cross-sectional study. J Cancer Surviv 8 (4): 688-96, 2014.
-
Krull KR, Khan RB, Ness KK, et al.: Symptoms of attention-deficit/hyperactivity disorder in long-term survivors of childhood leukemia. Pediatr Blood Cancer 57 (7): 1191-6, 2011.
-
Kahalley LS, Conklin HM, Tyc VL, et al.: ADHD and secondary ADHD criteria fail to identify many at-risk survivors of pediatric ALL and brain tumor. Pediatr Blood Cancer 57 (1): 110-8, 2011.
-
Reddick WE, Glass JO, Helton KJ, et al.: Prevalence of leukoencephalopathy in children treated for acute lymphoblastic leukemia with high-dose methotrexate. AJNR Am J Neuroradiol 26 (5): 1263-9, 2005.
-
Khong PL, Leung LH, Fung AS, et al.: White matter anisotropy in post-treatment childhood cancer survivors: preliminary evidence of association with neurocognitive function. J Clin Oncol 24 (6): 884-90, 2006.
-
Armstrong GT, Reddick WE, Petersen RC, et al.: Evaluation of memory impairment in aging adult survivors of childhood acute lymphoblastic leukemia treated with cranial radiotherapy. J Natl Cancer Inst 105 (12): 899-907, 2013.
-
Zeller B, Tamnes CK, Kanellopoulos A, et al.: Reduced neuroanatomic volumes in long-term survivors of childhood acute lymphoblastic leukemia. J Clin Oncol 31 (17): 2078-85, 2013.
-
Faraci M, Morana G, Bagnasco F, et al.: Magnetic resonance imaging in childhood leukemia survivors treated with cranial radiotherapy: a cross sectional, single center study. Pediatr Blood Cancer 57 (2): 240-6, 2011.
-
Reimers TS, Ehrenfels S, Mortensen EL, et al.: Cognitive deficits in long-term survivors of childhood brain tumors: Identification of predictive factors. Med Pediatr Oncol 40 (1): 26-34, 2003.
-
Palmer SL, Goloubeva O, Reddick WE, et al.: Patterns of intellectual development among survivors of pediatric medulloblastoma: a longitudinal analysis. J Clin Oncol 19 (8): 2302-8, 2001.
-
Merchant TE, Schreiber JE, Wu S, et al.: Critical combinations of radiation dose and volume predict intelligence quotient and academic achievement scores after craniospinal irradiation in children with medulloblastoma. Int J Radiat Oncol Biol Phys 90 (3): 554-61, 2014.
-
Armstrong GT, Conklin HM, Huang S, et al.: Survival and long-term health and cognitive outcomes after low-grade glioma. Neuro Oncol 13 (2): 223-34, 2011.
-
Di Pinto M, Conklin HM, Li C, et al.: Learning and memory following conformal radiation therapy for pediatric craniopharyngioma and low-grade glioma. Int J Radiat Oncol Biol Phys 84 (3): e363-9, 2012.
-
Ris MD, Walsh K, Wallace D, et al.: Intellectual and academic outcome following two chemotherapy regimens and radiotherapy for average-risk medulloblastoma: COG A9961. Pediatr Blood Cancer 60 (8): 1350-7, 2013.
-
Orgel E, O'Neil SH, Kayser K, et al.: Effect of Sensorineural Hearing Loss on Neurocognitive Functioning in Pediatric Brain Tumor Survivors. Pediatr Blood Cancer 63 (3): 527-34, 2016.
-
Bowers DC, Liu Y, Leisenring W, et al.: Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol 24 (33): 5277-82, 2006.
-
Mabbott DJ, Spiegler BJ, Greenberg ML, et al.: Serial evaluation of academic and behavioral outcome after treatment with cranial radiation in childhood. J Clin Oncol 23 (10): 2256-63, 2005.
-
Brière ME, Scott JG, McNall-Knapp RY, et al.: Cognitive outcome in pediatric brain tumor survivors: delayed attention deficit at long-term follow-up. Pediatr Blood Cancer 50 (2): 337-40, 2008.
-
Edelstein K, Spiegler BJ, Fung S, et al.: Early aging in adult survivors of childhood medulloblastoma: long-term neurocognitive, functional, and physical outcomes. Neuro Oncol 13 (5): 536-45, 2011.
-
Mulhern RK, Merchant TE, Gajjar A, et al.: Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol 5 (7): 399-408, 2004.
-
Mulhern RK, White HA, Glass JO, et al.: Attentional functioning and white matter integrity among survivors of malignant brain tumors of childhood. J Int Neuropsychol Soc 10 (2): 180-9, 2004.
-
Reddick WE, White HA, Glass JO, et al.: Developmental model relating white matter volume to neurocognitive deficits in pediatric brain tumor survivors. Cancer 97 (10): 2512-9, 2003.
-
Brinkman TM, Reddick WE, Luxton J, et al.: Cerebral white matter integrity and executive function in adult survivors of childhood medulloblastoma. Neuro Oncol 14 (Suppl 4): iv25-36, 2012.
-
Jacola LM, Ashford JM, Reddick WE, et al.: The relationship between working memory and cerebral white matter volume in survivors of childhood brain tumors treated with conformal radiation therapy. J Neurooncol 119 (1): 197-205, 2014.
-
Palmer SL, Glass JO, Li Y, et al.: White matter integrity is associated with cognitive processing in patients treated for a posterior fossa brain tumor. Neuro Oncol 14 (9): 1185-93, 2012.
-
Ris MD, Packer R, Goldwein J, et al.: Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children's Cancer Group study. J Clin Oncol 19 (15): 3470-6, 2001.
-
Kahalley LS, Ris MD, Grosshans DR, et al.: Comparing Intelligence Quotient Change After Treatment With Proton Versus Photon Radiation Therapy for Pediatric Brain Tumors. J Clin Oncol 34 (10): 1043-9, 2016.
-
Pulsifer MB, Sethi RV, Kuhlthau KA, et al.: Early Cognitive Outcomes Following Proton Radiation in Pediatric Patients With Brain and Central Nervous System Tumors. Int J Radiat Oncol Biol Phys 93 (2): 400-7, 2015.
-
Merchant TE, Conklin HM, Wu S, et al.: Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol 27 (22): 3691-7, 2009.
-
Palmer SL, Armstrong C, Onar-Thomas A, et al.: Processing speed, attention, and working memory after treatment for medulloblastoma: an international, prospective, and longitudinal study. J Clin Oncol 31 (28): 3494-500, 2013.
-
Knight SJ, Conklin HM, Palmer SL, et al.: Working memory abilities among children treated for medulloblastoma: parent report and child performance. J Pediatr Psychol 39 (5): 501-11, 2014.
-
Schreiber JE, Gurney JG, Palmer SL, et al.: Examination of risk factors for intellectual and academic outcomes following treatment for pediatric medulloblastoma. Neuro Oncol 16 (8): 1129-36, 2014.
-
Moxon-Emre I, Bouffet E, Taylor MD, et al.: Impact of craniospinal dose, boost volume, and neurologic complications on intellectual outcome in patients with medulloblastoma. J Clin Oncol 32 (17): 1760-8, 2014.
-
Armstrong GT, Liu Q, Yasui Y, et al.: Long-term outcomes among adult survivors of childhood central nervous system malignancies in the Childhood Cancer Survivor Study. J Natl Cancer Inst 101 (13): 946-58, 2009.
-
Brinkman TM, Palmer SL, Chen S, et al.: Parent-reported social outcomes after treatment for pediatric embryonal tumors: a prospective longitudinal study. J Clin Oncol 30 (33): 4134-40, 2012.
-
Moyer KH, Willard VW, Gross AM, et al.: The impact of attention on social functioning in survivors of pediatric acute lymphoblastic leukemia and brain tumors. Pediatr Blood Cancer 59 (7): 1290-5, 2012.
-
Mitby PA, Robison LL, Whitton JA, et al.: Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer 97 (4): 1115-26, 2003.
-
Kunin-Batson A, Kadan-Lottick N, Zhu L, et al.: Predictors of independent living status in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer 57 (7): 1197-203, 2011.
-
Janson C, Leisenring W, Cox C, et al.: Predictors of marriage and divorce in adult survivors of childhood cancers: a report from the Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev 18 (10): 2626-35, 2009.
-
Pui CH, Howard SC: Current management and challenges of malignant disease in the CNS in paediatric leukaemia. Lancet Oncol 9 (3): 257-68, 2008.
-
Waber DP, Queally JT, Catania L, et al.: Neuropsychological outcomes of standard risk and high risk patients treated for acute lymphoblastic leukemia on Dana-Farber ALL consortium protocol 95-01 at 5 years post-diagnosis. Pediatr Blood Cancer 58 (5): 758-65, 2012.
-
Krull KR, Brinkman TM, Li C, et al.: Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude lifetime cohort study. J Clin Oncol 31 (35): 4407-15, 2013.
-
Reddick WE, Shan ZY, Glass JO, et al.: Smaller white-matter volumes are associated with larger deficits in attention and learning among long-term survivors of acute lymphoblastic leukemia. Cancer 106 (4): 941-9, 2006.
-
Kadan-Lottick NS, Zeltzer LK, Liu Q, et al.: Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. J Natl Cancer Inst 102 (12): 881-93, 2010.
-
Krull KR, Zhang N, Santucci A, et al.: Long-term decline in intelligence among adult survivors of childhood acute lymphoblastic leukemia treated with cranial radiation. Blood 122 (4): 550-3, 2013.
-
Annett RD, Hile S, Bedrick E, et al.: Neuropsychological functioning of children treated for acute lymphoblastic leukemia: impact of whole brain radiation therapy. Psychooncology 24 (2): 181-9, 2015.
-
Schuitema I, Deprez S, Van Hecke W, et al.: Accelerated aging, decreased white matter integrity, and associated neuropsychological dysfunction 25 years after pediatric lymphoid malignancies. J Clin Oncol 31 (27): 3378-88, 2013.
-
Spiegler BJ, Kennedy K, Maze R, et al.: Comparison of long-term neurocognitive outcomes in young children with acute lymphoblastic leukemia treated with cranial radiation or high-dose or very high-dose intravenous methotrexate. J Clin Oncol 24 (24): 3858-64, 2006.
-
Campbell LK, Scaduto M, Sharp W, et al.: A meta-analysis of the neurocognitive sequelae of treatment for childhood acute lymphocytic leukemia. Pediatr Blood Cancer 49 (1): 65-73, 2007.
-
Mennes M, Stiers P, Vandenbussche E, et al.: Attention and information processing in survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only. Pediatr Blood Cancer 44 (5): 478-86, 2005.
-
Jansen NC, Kingma A, Schuitema A, et al.: Neuropsychological outcome in chemotherapy-only-treated children with acute lymphoblastic leukemia. J Clin Oncol 26 (18): 3025-30, 2008.
-
Iyer NS, Balsamo LM, Bracken MB, et al.: Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood 126 (3): 346-53, 2015.
-
Jacola LM, Krull KR, Pui CH, et al.: Longitudinal Assessment of Neurocognitive Outcomes in Survivors of Childhood Acute Lymphoblastic Leukemia Treated on a Contemporary Chemotherapy Protocol. J Clin Oncol 34 (11): 1239-47, 2016.
-
Espy KA, Moore IM, Kaufmann PM, et al.: Chemotherapeutic CNS prophylaxis and neuropsychologic change in children with acute lymphoblastic leukemia: a prospective study. J Pediatr Psychol 26 (1): 1-9, 2001 Jan-Feb.
-
Kaemingk KL, Carey ME, Moore IM, et al.: Math weaknesses in survivors of acute lymphoblastic leukemia compared to healthy children. Child Neuropsychol 10 (1): 14-23, 2004.
-
Buizer AI, de Sonneville LM, Veerman AJ: Effects of chemotherapy on neurocognitive function in children with acute lymphoblastic leukemia: a critical review of the literature. Pediatr Blood Cancer 52 (4): 447-54, 2009.
-
von der Weid N, Mosimann I, Hirt A, et al.: Intellectual outcome in children and adolescents with acute lymphoblastic leukaemia treated with chemotherapy alone: age- and sex-related differences. Eur J Cancer 39 (3): 359-65, 2003.
-
Krull KR, Cheung YT, Liu W, et al.: Chemotherapy Pharmacodynamics and Neuroimaging and Neurocognitive Outcomes in Long-Term Survivors of Childhood Acute Lymphoblastic Leukemia. J Clin Oncol 34 (22): 2644-53, 2016.
-
Conklin HM, Krull KR, Reddick WE, et al.: Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst 104 (18): 1386-95, 2012.
-
Halsey C, Buck G, Richards S, et al.: The impact of therapy for childhood acute lymphoblastic leukaemia on intelligence quotients; results of the risk-stratified randomized central nervous system treatment trial MRC UKALL XI. J Hematol Oncol 4: 42, 2011.
-
Kadan-Lottick NS, Brouwers P, Breiger D, et al.: A comparison of neurocognitive functioning in children previously randomized to dexamethasone or prednisone in the treatment of childhood acute lymphoblastic leukemia. Blood 114 (9): 1746-52, 2009.
-
Edelmann MN, Daryani VM, Bishop MW, et al.: Neurocognitive and Patient-Reported Outcomes in Adult Survivors of Childhood Osteosarcoma. JAMA Oncol 2 (2): 201-8, 2016.
-
Phipps S, Rai SN, Leung WH, et al.: Cognitive and academic consequences of stem-cell transplantation in children. J Clin Oncol 26 (12): 2027-33, 2008.
-
Shah AJ, Epport K, Azen C, et al.: Progressive declines in neurocognitive function among survivors of hematopoietic stem cell transplantation for pediatric hematologic malignancies. J Pediatr Hematol Oncol 30 (6): 411-8, 2008.
-
Anderson FS, Kunin-Batson AS, Perkins JL, et al.: White versus gray matter function as seen on neuropsychological testing following bone marrow transplant for acute leukemia in childhood. Neuropsychiatr Dis Treat 4 (1): 283-8, 2008.
-
Jain P, Gulati S, Seth R, et al.: Vincristine-induced neuropathy in childhood ALL (acute lymphoblastic leukemia) survivors: prevalence and electrophysiological characteristics. J Child Neurol 29 (7): 932-7, 2014.
-
Ness KK, Hudson MM, Pui CH, et al.: Neuromuscular impairments in adult survivors of childhood acute lymphoblastic leukemia: associations with physical performance and chemotherapy doses. Cancer 118 (3): 828-38, 2012.
-
Ness KK, Jones KE, Smith WA, et al.: Chemotherapy-related neuropathic symptoms and functional impairment in adult survivors of extracranial solid tumors of childhood: results from the St. Jude Lifetime Cohort Study. Arch Phys Med Rehabil 94 (8): 1451-7, 2013.
-
Goldsby RE, Liu Q, Nathan PC, et al.: Late-occurring neurologic sequelae in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol 28 (2): 324-31, 2010.
-
Hörnquist L, Rickardsson J, Lannering B, et al.: Altered self-perception in adult survivors treated for a CNS tumor in childhood or adolescence: population-based outcomes compared with the general population. Neuro Oncol 17 (5): 733-40, 2015.
-
Schulte F, Barrera M: Social competence in childhood brain tumor survivors: a comprehensive review. Support Care Cancer 18 (12): 1499-513, 2010.
-
Brinkman TM, Krasin MJ, Liu W, et al.: Long-Term Neurocognitive Functioning and Social Attainment in Adult Survivors of Pediatric CNS Tumors: Results From the St Jude Lifetime Cohort Study. J Clin Oncol 34 (12): 1358-67, 2016.
-
Brinkman TM, Zhu L, Zeltzer LK, et al.: Longitudinal patterns of psychological distress in adult survivors of childhood cancer. Br J Cancer 109 (5): 1373-81, 2013.
-
Brinkman TM, Zhang N, Recklitis CJ, et al.: Suicide ideation and associated mortality in adult survivors of childhood cancer. Cancer 120 (2): 271-7, 2014.
-
Sun CL, Francisco L, Baker KS, et al.: Adverse psychological outcomes in long-term survivors of hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study (BMTSS). Blood 118 (17): 4723-31, 2011.
-
Fuemmeler BF, Elkin TD, Mullins LL: Survivors of childhood brain tumors: behavioral, emotional, and social adjustment. Clin Psychol Rev 22 (4): 547-85, 2002.
-
Recklitis C, O'Leary T, Diller L: Utility of routine psychological screening in the childhood cancer survivor clinic. J Clin Oncol 21 (5): 787-92, 2003.
-
Phipps S, Klosky JL, Long A, et al.: Posttraumatic stress and psychological growth in children with cancer: has the traumatic impact of cancer been overestimated? J Clin Oncol 32 (7): 641-6, 2014.
-
Phipps S, Larson S, Long A, et al.: Adaptive style and symptoms of posttraumatic stress in children with cancer and their parents. J Pediatr Psychol 31 (3): 298-309, 2006.
-
Phipps S, Jurbergs N, Long A: Symptoms of post-traumatic stress in children with cancer: does personality trump health status? Psychooncology 18 (9): 992-1002, 2009.
-
Stuber ML, Meeske KA, Leisenring W, et al.: Defining medical posttraumatic stress among young adult survivors in the Childhood Cancer Survivor Study. Gen Hosp Psychiatry 33 (4): 347-53, 2011 Jul-Aug.
-
Rourke MT, Hobbie WL, Schwartz L, et al.: Posttraumatic stress disorder (PTSD) in young adult survivors of childhood cancer. Pediatr Blood Cancer 49 (2): 177-82, 2007.
-
Schwartz L, Drotar D: Posttraumatic stress and related impairment in survivors of childhood cancer in early adulthood compared to healthy peers. J Pediatr Psychol 31 (4): 356-66, 2006.
-
Stuber ML, Meeske KA, Krull KR, et al.: Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics 125 (5): e1124-34, 2010.
-
Hobbie WL, Stuber M, Meeske K, et al.: Symptoms of posttraumatic stress in young adult survivors of childhood cancer. J Clin Oncol 18 (24): 4060-6, 2000.
-
Dieluweit U, Debatin KM, Grabow D, et al.: Social outcomes of long-term survivors of adolescent cancer. Psychooncology 19 (12): 1277-84, 2010.
-
Seitz DC, Hagmann D, Besier T, et al.: Life satisfaction in adult survivors of cancer during adolescence: what contributes to the latter satisfaction with life? Qual Life Res 20 (2): 225-36, 2011.
-
Tai E, Buchanan N, Townsend J, et al.: Health status of adolescent and young adult cancer survivors. Cancer 118 (19): 4884-91, 2012.
-
Schultz KA, Ness KK, Whitton J, et al.: Behavioral and social outcomes in adolescent survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 25 (24): 3649-56, 2007.
-
Prasad PK, Hardy KK, Zhang N, et al.: Psychosocial and Neurocognitive Outcomes in Adult Survivors of Adolescent and Early Young Adult Cancer: A Report From the Childhood Cancer Survivor Study. J Clin Oncol 33 (23): 2545-52, 2015.
-
Krull KR, Huang S, Gurney JG, et al.: Adolescent behavior and adult health status in childhood cancer survivors. J Cancer Surviv 4 (3): 210-7, 2010.
-
Freyer DR: Transition of care for young adult survivors of childhood and adolescent cancer: rationale and approaches. J Clin Oncol 28 (32): 4810-8, 2010.
-
Nathan PC, Hayes-Lattin B, Sisler JJ, et al.: Critical issues in transition and survivorship for adolescents and young adults with cancers. Cancer 117 (10 Suppl): 2335-41, 2011.
Late Effects of the Digestive SystemDental Overview Chemotherapy, radiation therapy, and local surgery can cause multiple cosmetic and functional abnormalities of the oral cavity and dentition. The quality of current evidence regarding this outcome is limited by retrospective data collection, small sample size, cohort selection and participation bias, and heterogeneity in treatment approach, time since treatment, and method of ascertainment. Oral and dental complications reported in childhood cancer survivors include the following: - Abnormalities of tooth development.
- Salivary gland dysfunction.
- Abnormalities of craniofacial development.
Abnormalities of tooth development Abnormalities of dental development reported in childhood cancer survivors include absence of tooth development, hypodontia, microdontia, enamel hypoplasia, and root malformation.[1,2,3,4,5,6,7,8,9] The prevalence of hypodontia has varied widely in series depending on age at diagnosis, treatment modality, and method of ascertainment. Cancer treatments that have been associated with dental maldevelopment include head and neck radiation therapy, any chemotherapy, and hematopoietic stem cell transplantation (HSCT). Children younger than 5 years are at greatest risk for dental anomalies, such as root agenesis, delayed eruption, enamel defects, and/or excessive caries related to disruption of ameloblast (enamel producing) and odontoblast (dentin producing) activity early in life.[3] Key findings related to cancer treatment effect on tooth development include the following: - Radiation directed at oral cavity or surrounding structures increases the risk of dental anomalies because ameloblasts can be permanently damaged by doses as low as 10 Gy.[3,5,6,10] However, the most significant degree of tooth aplasia or delayed eruption occurs in younger children (aged <4 years) who are exposed to radiation doses of 20 Gy or higher.[11] Developing teeth may be irradiated in the course of treating head and neck sarcomas, Hodgkin lymphoma, neuroblastoma, central nervous system leukemia, nasopharyngeal cancer, and as a component of total-body irradiation (TBI). Doses of 10 Gy to 40 Gy can cause root shortening or abnormal curvature, dwarfism, and hypocalcification.[12] Significant dental abnormalities, including mandibular or maxillary hypoplasia, increased caries, hypodontia, microdontia, root stunting, and xerostomia have been reported in more than 85% of survivors of head and neck rhabdomyosarcoma treated with radiation doses higher than 40 Gy.[4,5]
- Chemotherapy, especially exposure to alkylating agents, can affect tooth development.[3,6,7] Chemotherapy for the treatment of leukemia can cause shortening and thinning of the premolar roots and enamel abnormalities.[13,14,15] Childhood Cancer Survivor Study (CCSS) investigators identified age younger than 5 years and increased exposure to cyclophosphamide as significant risk factors for developmental dental abnormalities in long-term survivors of childhood cancer.[3]
- HSCT conditioning, especially regimens containing TBI, may result in tooth agenesis and root malformation. Younger children who have not developed secondary teeth are most vulnerable.[1,2,6] Children who undergo HSCT with TBI may develop short V-shaped roots, microdontia, enamel hypoplasia, and/or premature apical closure.[1,2,8] The younger a patient is when treated with HSCT, the more severely disturbed dental development will be and the more deficient vertical growth of the lower face will be. These high-risk patients require close surveillance and appropriate interventions.[9]
Salivary gland dysfunction Xerostomia, the sensation of dry mouth, is a potential side effect following head and neck irradiation or HSCT that can severely impact quality of life. Complications of reduced salivary secretion include increased caries, susceptibility to oral infections, sleep disturbances, and difficulties with chewing, swallowing, and speaking.[16,17] The prevalence of salivary gland dysfunction after cancer treatment varies based on measurement techniques (patient report vs. stimulated or unstimulated salivary secretion rates).[18] In general, the prevalence of self-reported persistent posttherapy xerostomia is infrequent among childhood cancer survivors. In the CCSS, the prevalence of self-reported xerostomia in survivors was 2.8 % compared with 0.3% in siblings, with an increased risk in survivors older than 30 years.[3] - Salivary gland irradiation incidental to treatment of head and neck malignancies or Hodgkin lymphoma causes a qualitative and quantitative change in salivary flow, which can be reversible after doses of less than 40 Gy but may be irreversible after higher doses, depending on whether sensitizing chemotherapy is also administered.[16]
- The association of chemotherapy alone with xerostomia remains controversial.[16] Only one study of pediatric patients demonstrated an excess risk (odds ratio, 12.32 [2.1-74.4]) of decreased stimulated saliva flow rates among patients treated with cyclophosphamide; however, no increased dental caries were noted and patient-reported xerostomia was not evaluated.[7]
- HSCT recipients are at increased risk of salivary gland dysfunction related to transplant conditioning or graft-versus-host disease (GVHD). GVHD can cause hyposalivation and xerostomia with resultant dental disease. In a study of pediatric HSCT survivors, 60% of those exposed to a conditioning regimen with cyclophosphamide and 10 Gy single-dose TBI had decreased salivary secretion rates, compared with 26% in those who received cyclophosphamide and busulfan.[19] In contrast, in another study, the prevalence of reduced salivary secretion did not differ among long-term survivors based on conditioning regimen (single-dose TBI, 47%; fractionated TBI, 47%; busulfan, 42%).[20]
- The impact of infectious complications and alterations in the microflora during and after therapy is not known.[6]
Abnormalities of craniofacial development Craniofacial maldevelopment is a common adverse outcome among children treated with high-dose radiation therapy to the head and neck that frequently occurs in association with other oral cavity sequelae such as dental anomalies, xerostomia, and trismus.[5,21,22] The extent and severity of musculoskeletal disfigurement is related to age at treatment and radiation therapy volume and dose, with higher risk observed among younger patients and those who received 30 Gy or more. Remediation of cosmetic and functional abnormalities often requires multiple surgical interventions. Posttherapy management Some studies suggest there may be a benefit of fluoride products or chlorhexidine rinses in patients who have undergone radiation therapy.[23] Dental caries are a problematic consequence of reduced salivary quality and flow. The use of topical fluoride can dramatically reduce the frequency of caries, and saliva substitutes and sialagogues can ameliorate sequelae such as xerostomia.[17] It has been reported that the incidence of dental visits for childhood cancer survivors falls below the American Dental Association's recommendation that all adults visit the dentist annually.[24] The Children's Oncology Group Long-term Follow-Up Guidelines recommend biannual dental cleaning and exams for all survivors of childhood cancer. These findings give health care providers further impetus to encourage routine dental care and dental hygiene evaluations for survivors of childhood treatment. (Refer to the PDQ summary on Oral Complications of Chemotherapy and Head/Neck Radiation for more information about oral complications in cancer patients.) Table 4. Oral/Dental Late Effectsa| Predisposing Therapy | Oral/Dental Effects | Health Screening/Interventions |
|---|
| CT = computed tomography; GVHD = graft-versus-host disease; MRI = magnetic resonance imaging. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Any chemotherapy; radiation impacting oral cavity | Dental developmental abnormalities; tooth/root agenesis; microdontia; root thinning/shortening; enamel dysplasia | Dental evaluation and cleaning every 6 months | | Regular dental care including fluoride applications | | Consultation with orthodontist experienced in management of irradiated childhood cancer survivors | | Baseline panorex before dental procedures to evaluate root development | | Radiation impacting oral cavity | Malocclusion; temporomandibular joint dysfunction | Dental evaluation and cleaning every 6 months | | Regular dental care including fluoride applications | | Consultation with orthodontist experienced in management of irradiated childhood cancer survivors | | Baseline panorex before dental procedures to evaluate root development | | Radiation impacting oral cavity; hematopoietic cell transplantation with history of chronic GVHD | Xerostomia/salivary gland dysfunction; periodontal disease; dental caries; oral cancer (squamous cell carcinoma) | Dental evaluation and cleaning every 6 months | | Supportive care with saliva substitutes, moistening agents, and sialogogues (pilocarpine) | | Regular dental care including fluoride applications | | Radiation impacting oral cavity (≥40 Gy) | Osteoradionecrosis | History: impaired or delayed healing after dental work | | Exam: persistent jaw pain, swelling or trismus | | Imaging studies (x-ray, CT scan and/or MRI) may assist in making diagnosis | | Surgical biopsy may be needed to confirm diagnosis | | Consider hyperbaric oxygen treatments | Digestive Tract Overview The gastrointestinal (GI) tract is sensitive to the acute toxicities of chemotherapy, radiation therapy, and surgery. However, these important treatment modalities can also result in some long-term issues in a treatment- and dose-dependent manner. Reports published about long-term GI tract outcomes are limited by retrospective data collection, small sample size, cohort selection and participation bias, heterogeneity in treatment approach, time since treatment, and method of ascertainment. Key concepts about GI complications observed in childhood cancer survivors include the following: - Treatment-related late effects include the following:
- Cancer and its therapy can increase the risk of upper and lower digestive tract late effects.
- Dose intensity of chemotherapy and use of abdominal irradiation influences the risk of digestive tract late effects.
- Abdominal surgery increases risk of adhesions and predisposes patients to postoperative bowel obstruction.
- Digestive tract-related late effects include the following:
- Esophageal dysmotility.
- Gastroesophageal reflux.
- Gastritis, enteritis, or colitis.
- GI motility dysfunction (diarrhea, constipation, bowel obstruction).
- Subsequent malignant neoplasms
GI outcomes from selected cohort studies GI outcomes from selected cohort studies include the following: - Among 5-year childhood cancer survivors participating in the CCSS, the cumulative incidence of self-reported GI conditions was 37.6% at 20 years (25.8% for upper GI complications and 15.5% for lower GI complications) from cancer diagnosis, representing an almost twofold excess risk of upper GI complications (relative risk [RR], 1.8; 95% confidence interval [CI], 1.6-2.0) and lower GI complications (RR, 1.9; 95% CI, 1.7-2.2), compared with sibling controls. Factors predicting higher risk of specific GI complications include the following:[25]
- Older age at diagnosis.
- Intensified therapy (anthracyclines for upper GI complications and alkylating agents for lower GI complications).
- Abdominal radiation therapy.
- Abdominal surgery.
- Another cohort study of children treated for acute myeloid leukemia with chemotherapy alone found that reported GI disorders were relatively rare and not significantly different from those reported by sibling controls.[26]
- Late radiation injury to the digestive tract is attributable to vascular injury. Necrosis, ulceration, stenosis, or perforation can occur and are characterized by malabsorption, pain, and recurrent episodes of bowel obstruction, as well as perforation and infection.[27,28,29] In general, fractionated doses of 20 Gy to 30 Gy can be delivered to the small bowel without significant long-term morbidity. Doses greater than 40 Gy cause bowel obstruction or chronic enterocolitis.[30] Sensitizing chemotherapeutic agents such as dactinomycin or anthracyclines can increase this risk.
Impact of cancer histology on GI outcomes Intra-abdominal tumors represent a relatively common location for several pediatric malignancies, including rhabdomyosarcoma, Wilms tumor, lymphoma, germ cell tumors, and neuroblastoma. Intra-abdominal tumors often require multimodal therapy, occasionally necessitating resection of bowel and bowel-injuring chemotherapy and/or radiation therapy. Thus, these tumors would be expected to be particularly prone to long-term digestive tract issues. A limited number of reports describe GI complications in pediatric patients with genitourinary solid tumors treated with radiation therapy:[31,32,33,34,35] - One study comprehensively evaluated intestinal symptoms in 44 children with cancer who underwent whole-abdominal (10-40 Gy) and involved-field (25-40 Gy) radiation therapy and received additional interventions predisposing them to GI tract complications including abdominal laparotomy in 43 patients (98%) and chemotherapy in 25 patients (57%).[31] Late small-bowel obstruction was observed in 36% of patients surviving for 19 months to 7 years, which was uniformly preceded by small bowel toxicity during therapy.
- The CCSS evaluated the incidence and risk of late-occurring intestinal obstruction requiring surgery in 12,316 5-year survivors (2,002 with and 10,314 without abdominopelvic tumors) and 4,023 siblings. The most common diagnoses among survivors with abdominopelvic tumors were Wilms tumors and neuroblastomas but also included soft tissue sarcomas, lymphomas, and bone tumors. The cumulative incidence of late intestinal obstruction requiring surgery at 35 years was 5.8% among survivors with abdominopelvic tumors, 1.0% among those without abdominopelvic tumors, and 0.3% among siblings. Elevated risk of intestinal obstruction requiring surgery was associated with presence of an abdominopelvic tumor (adjusted rate ratio [ARR], 3.6; P < .001) and exposure to abdominal or pelvic radiation therapy within 5 years of cancer diagnosis (ARR, 2.4; P < .001). Among survivors of abdominopelvic tumors, the median time from diagnosis to the first late intestinal obstruction requiring surgery was 12 years (range, 8-19 years). Lymphoma resulted in the highest cumulative incidence of late-occurring intestinal obstruction requiring surgery (7.2% at 35 years after diagnosis). An elevated risk of obstruction was associated with the presence of an abdominopelvic tumor and previous exposure to abdominal or pelvic radiation therapy.[36][Level of evidence: 3iiiC]
- Reports from the Intergroup Rhabdomyosarcoma Study evaluating GI toxicity in long-term survivors of genitourinary rhabdomyosarcoma infrequently observed abnormalities of the irradiated bowel.[32,33,35] Radiation-related complications occurred in approximately 10% of long-term survivors of paratesticular and bladder/prostate rhabdomyosarcoma and included intraperitoneal adhesions with bowel obstruction, chronic diarrhea, and stricture or enteric fistula formation.[32,35]
Table 5. Digestive Tract Late Effectsa| Predisposing Therapy | Gastrointestinal Effects | Health Screening/Interventions |
|---|
| GVHD = graft-versus-host disease; KUB = kidneys, ureter, bladder (plain abdominal radiograph). | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Radiation impacting esophagus; hematopoietic cell transplantation with any history of chronic GVHD | Esophageal stricture | History: dysphagia, heart burn | | Esophageal dilation, antireflux surgery | | Radiation impacting bowel | Chronic enterocolitis; fistula; strictures | History: nausea, vomiting, abdominal pain, diarrhea | | Serum protein and albumin levels yearly in patients with chronic diarrhea or fistula | | Surgical and/or gastroenterology consultation for symptomatic patients | | Radiation impacting bowel; laparotomy | Bowel obstruction | History: abdominal pain, distention, vomiting, constipation | | Exam: tenderness, abdominal guarding, distension (acute episode) | | Obtain KUB in patients with clinical symptoms of obstruction | | Surgical consultation in patients unresponsive to medical management | | Pelvic surgery; cystectomy | Fecal incontinence | History: chronic constipation, fecal soiling | | Rectal exam | Hepatobiliary Complications Overview Hepatic complications resulting from childhood cancer therapy are observed primarily as acute treatment toxicities.[37] Because many chemotherapy agents and radiation are hepatotoxic, transient liver function anomalies are common during therapy. Severe acute hepatic complications occur rarely. Survivors of childhood cancer can occasionally exhibit long-standing hepatic injury. Some general concepts regarding hepatotoxicity related to childhood cancer include the following: - The risk of long-term hepatotoxicity is not well defined.
- Children with primary liver tumors requiring significant liver resection, or even transplant, are at higher risk for liver injury.
- Children receiving radiation therapy to the liver are at higher risk for liver injury.
- Children undergoing bone marrow transplant are at higher risk for liver injury.
Certain factors, including the type of chemotherapy, the dose and extent of radiation exposure, the influence of surgical interventions, and the evolving impact of viral hepatitis and/or other infectious complication, need additional attention in future studies. Types of hepatobiliary complications - Asymptomatic elevations of blood biomarkers. Blood biomarkers include the following: serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyltransferase (GGT). Liver injury related to treatment for childhood cancer is often asymptomatic and indolent in course. Dutch investigators observed hepatobiliary dysfunction in 8.7% of 1,362 long-term survivors (median follow-up, 12.4 years since diagnosis) evaluated by ALT for hepatocellular injury and GGT for biliary tract injury. Cases with a history of viral hepatitis and a history of veno-occlusive disease were excluded. Predictors for elevated ALT and GGT by multivariable analysis included treatment with radiation therapy involving the liver, higher body mass index (BMI), higher alcohol intake, and longer follow-up time; older age at diagnosis was only significantly associated with elevated GGT levels.[38] In a CCSS report, survivors of childhood cancer were more than two times more likely to report a hepatic-related health issue and were nearly nine times more likely to report cirrhosis, compared with sibling controls.[25]
Less commonly reported hepatobiliary complications include the following: - Cholelithiasis. In limited studies, an increased risk of cholelithiasis has been linked to ileal conduit, parenteral nutrition, abdominal surgery, abdominal radiation therapy, and HSCT.[39,40] Gallbladder disease was the most frequent late-onset liver condition reported among participants in the CCSS, and they had a twofold excess risk compared with sibling controls (RR, 2.0; 95% CI, 2.0-40.0).[25]
- Focal nodular hyperplasia. Lesions made up of regenerating liver called focal nodular hyperplasia have been incidentally noted after chemotherapy or HSCT.[41,42] These lesions are thought to be iatrogenic manifestations of vascular damage and have been associated with veno-occlusive disease, high-dose alkylating agents (e.g., busulfan and melphalan), and liver irradiation. The prevalence of this finding is unknown; while noted at less than 1% in some papers,[42] this is likely an underestimate. In one study of patients who were followed by magnetic resonance imaging (MRI) after transplant to assess liver iron stores, the cumulative incidence was 35% at 150 months posttransplant.[41] The lesions can mimic metastatic or subsequent tumors, but MRI imaging is generally diagnostic, and unless the lesions grow or patients have worrisome symptoms, biopsy or resection is generally not necessary.
- Nodular regenerative hyperplasia. Nodular regenerative hyperplasia is a rare condition characterized by the development of multiple monoacinar regenerative hepatic nodules and mild fibrosis. The pathogenesis is not well established but may represent a nonspecific tissue adaptation to heterogeneous hepatic blood flow.[43] Nodular regenerative hyperplasia has rarely been observed in survivors of childhood cancer treated with chemotherapy, with or without liver irradiation.[44,45] Biopsy may be necessary to distinguish nodular regenerative hyperplasia from a subsequent malignancy.
- Microvesicular fatty change. In a cohort who recently completed intensified therapy for acute lymphoblastic leukemia, histologic evidence of fatty infiltration was noted in 93% and siderosis in up to 70% of patients.[46] Fibrosis developed in 11% and was associated with higher serum low-density lipoprotein (LDL) cholesterol. Fatty liver with insulin resistance has also been reported to develop more frequently in long-term childhood cancer survivors treated with cranial radiation therapy before allogeneic stem cell transplantation who were not overweight or obese.[47] Prospective studies are needed to define whether acute posttherapy fatty liver change contributes to the development of steatohepatitis or the metabolic syndrome in this population.
- Transfusion-related iron overload. Red blood cell transfusions can result in an accumulation of excess iron due to disruption of the homeostasis of iron storage and distribution when exogenous iron is loaded into organs. Transfusional iron overload has been reported in pediatric oncology patients, but its prevalence, organ distribution, and severity remain incompletely characterized. MRI has emerged as an accurate, noninvasive means for measuring iron in multiple organ systems.[48,49] In a cross-sectional study of 75 patients (4.4 years of median follow-up time; 4.9 years since last transfusion), MRI iron concentrations were elevated in the liver (49.3%) and pancreas (26.4%), but not in the heart. In a multivariable analysis, cumulative packed red blood cell volume and older age at diagnosis predicted elevated liver iron concentration.[48] Further research is needed to better characterize survivors at risk of clinically significant transfusion-related iron overload who may benefit from interventions to reduce iron loading and organ dysfunction.
Treatment-related risk factors for hepatobiliary complications The type and intensity of previous therapy influences risk for late-occurring hepatobiliary complications. In addition to the risk of treatment-related toxicity, recipients of HSCT frequently experience chronic liver dysfunction related to microvascular, immunologic, infectious, metabolic, and other toxic etiologies. - Chemotherapy. Chemotherapeutic agents with established hepatotoxic potential include antimetabolite agents like 6-mercaptopurine, 6-thioguanine, methotrexate, and rarely, dactinomycin. Veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) and cholestatic disease have been observed after thiopurine administration, especially 6-thioguanine. Progressive fibrosis and portal hypertension has been reported in a subset of children who developed VOD/SOS after treatment with 6-thioguanine.[50,51,52] Acute, dose-related, reversible VOD/SOS has been observed in children treated with dactinomycin for pediatric solid tumors.[53,54]
In the transplant setting, VOD/SOS has also been observed after conditioning regimens that have included cyclophosphamide/TBI, busulfan/cyclophosphamide and carmustine/cyclophosphamide/etoposide.[55] Because high-dose cyclophosphamide is common to all of these regimens, toxic cyclophosphamide metabolites resulting from the agent's variable metabolism have been speculated as a causative factor. - Radiation therapy. Acute radiation-induced liver disease also causes endothelial cell injury that is characteristic of VOD/SOS.[56] In adults, the whole liver has tolerance up to 30 Gy to 35 Gy with conventional fractionation, the prevalence of radiation-induced liver disease varies from 6% to 66% based on the volume of liver involved and on hepatic reserve.[56,57]
Based on limited data from pediatric cohorts treated in the 1970s and 1980s, persistent radiation hepatopathy after contemporary treatment appears to be uncommon in long-term survivors without predisposing conditions such as viral hepatitis or iron overload.[58] The risk of injury in children increases with radiation dose, hepatic volume, younger age at treatment, previous partial hepatectomy, and concomitant use of radiomimetic chemotherapy like dactinomycin and doxorubicin.[59,60,61,62] Survivors who received radiation doses of 40 Gy to at least one-third of liver volume, doses of 30 Gy or more to whole abdomen, or an upper abdominal field involving the entire liver are at highest risk for hepatic dysfunction.[63] - Hematopoietic stem cell transplantation. Chronic liver dysfunction in patients undergoing HSCT is multifactorial in etiology. The most common etiologies for chronic liver dysfunction include iron overload, chronic GVHD, and viral hepatitis.[64] Patients with chronic GVHD of the GI tract who exhibit an elevated bilirubin have a worse prognosis and quality of life.[65] While chronic liver dysfunction may be seen in more than half of long-term stem cell transplantation survivors, the course of the disease is mild and indolent in most patients.[66]
Infectious risk factors for hepatobiliary complications Viral hepatitis B and C may complicate the treatment course of childhood cancer and result in chronic hepatic dysfunction. Hepatitis B tends to have a more aggressive acute clinical course and a lower rate of chronic infection. Hepatitis C is characterized by a mild acute infection and a high rate of chronic infection. The incidence of transfusion-related hepatitis C in childhood cancer survivors has ranged from 5% to 50% depending on the geographic location of the reporting center.[67,68,69,70,71,72,73] Chronic hepatitis predisposes the childhood cancer survivor to cirrhosis, end-stage liver disease, and hepatocellular carcinoma. Concurrent infection with both viruses accelerates the progression of liver disease. Because most patients received some type of blood product during childhood cancer treatment and many are unaware of their transfusion history, screening based on date of diagnosis/treatment is recommended unless there is absolute certainty that the patient did not receive any blood or blood products.[74] Therefore, all children who received blood transfusions before 1972 should be screened for hepatitis B, and all children who received blood transfusions before 1993 should be screened for hepatitis C and referred for discussion of treatment options. Posttherapy management Survivors with liver dysfunction should be counseled regarding risk-reduction methods to prevent hepatic injury. Standard recommendations include maintenance of a healthy body weight, abstinence from alcohol use, and immunization against hepatitis A and B viruses. In patients with chronic hepatitis, precautions to reduce viral transmission to household and sexual contacts should also be reviewed. Table 6. Hepatobiliary Late Effectsa| Predisposing Therapy | Hepatic Effects | Health Screening/Interventions |
|---|
| ALT = alanine aminotransferase; AST = aspartate aminotransferase; HSCT = hematopoietic stem cell transplantation. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Methotrexate; mercaptopurine/thioguanine; HSCT | Hepatic dysfunction | Lab: ALT, AST, bilirubin levels | | Ferritin in those treated with HSCT | | Mercaptopurine/thioguanine; HSCT | Veno-occlusive disease/sinusoidal obstructive syndrome | Exam: scleral icterus, jaundice, ascites, hepatomegaly, splenomegaly | | Lab: ALT, AST, bilirubin, platelet levels | | Ferritin in those treated with HSCT | | Radiation impacting liver/biliary tract; HSCT | Hepatic fibrosis/cirrhosis | Exam: jaundice, spider angiomas, palmar erythema, xanthomata hepatomegaly, splenomegaly | | Lab: ALT, AST, bilirubin levels | | Ferritin in those treated with HSCT | | Prothrombin time for evaluation of hepatic synthetic function in patients with abnormal liver screening tests | | Screen for viral hepatitis in patients with persistently abnormal liver function or any patient transfused before 1993 | | Gastroenterology/hepatology consultation in patients with persistent liver dysfunction | | Hepatitis A and B immunizations in patients lacking immunity | | Consider phlebotomy and chelation therapy for iron overload | | Radiation impacting liver/biliary tract | Cholelithiasis | History: colicky abdominal pain related to fatty food intake, excessive flatulence | | Exam: right upper quadrant or epigastric tenderness (acute episode) | | Consider gallbladder ultrasound in patients with chronic abdominal pain | Pancreas The pancreas has been thought to be relatively radioresistant because of a paucity of information about late pancreatic-related effects. However, children and young adults treated with TBI or abdominal irradiation are known to have an increased risk of insulin resistance and diabetes mellitus.[75,76,77] A summary of the results of selected cancer cohort studies supporting this association include the following: - A retrospective cohort study, based on self-reports of 2,520 5-year survivors of childhood cancer treated in France and the United Kingdom, investigated the relationship between radiation dose to the pancreas and risk of a subsequent diabetes mellitus diagnosis. Sixty-five cases of diabetes mellitus were validated; the risk increased with radiation therapy to the tail of the pancreas, where the islets of Langerhans are concentrated. Risk increased up to 20 to 29 Gy and then plateaued. The estimated RR at 1 Gy was 1.61. Radiation dose to other parts of the pancreas did not have a significant effect. Compared with patients who did not receive radiation therapy, the RR of diabetes mellitus was 11.5 in patients who received more than 10 Gy to the pancreas. Children younger than 2 years at the time of radiation therapy were more sensitive than were older patients (RR at 1 Gy was 2.1 for the young age group vs. 1.4 for older patients). For the 511 patients who received more than 10 Gy, the cumulative incidence of diabetes mellitus was 16%.[78]
- Another study evaluated the risk of diabetes mellitus in 2,264 5-year survivors of Hodgkin lymphoma (42% younger than 25 years at diagnosis) After a median follow-up of 21.5 years, the cumulative incidence of diabetes mellitus was 8.3% (95% CI, 6.9%-9.8%) for the overall cohort and 14.2% (95% CI, 10.7%-18.3%) for those treated with more than 36 Gy para-aortic radiation. Survivors treated with more than 36 Gy of radiation to the para-aortic lymph nodes and spleen had a 2.3-fold increased risk of diabetes mellitus compared with those who did not receive radiation therapy. The risk of diabetes mellitus increased with higher doses to the pancreatic tail.[79]
- In a report from the CCSS that compared 8,599 childhood cancer survivors to 2,936 randomly selected sibling controls, and after adjustment for age, BMI, and several demographic factors, the risk of diabetes mellitus was 1.8 times higher in survivors (95% CI, 1.3-2.5; P < .001). Significant associations were found between diabetes mellitus and young age at diagnosis (0-4 years), the use of alkylating agents, and TBI or abdominal irradiation. Also, survivors were significantly more likely to be receiving medication for hypertension, dyslipidemia, and/or diabetes mellitus than were sibling controls.[80]
Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for digestive system late effects information including risk factors, evaluation, and health counseling. References:
-
Hölttä P, Alaluusua S, Saarinen-Pihkala UM, et al.: Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer 103 (1): 181-90, 2005.
-
Hölttä P, Hovi L, Saarinen-Pihkala UM, et al.: Disturbed root development of permanent teeth after pediatric stem cell transplantation. Dental root development after SCT. Cancer 103 (7): 1484-93, 2005.
-
Kaste SC, Goodman P, Leisenring W, et al.: Impact of radiation and chemotherapy on risk of dental abnormalities: a report from the Childhood Cancer Survivor Study. Cancer 115 (24): 5817-27, 2009.
-
Paulino AC: Role of radiation therapy in parameningeal rhabdomyosarcoma. Cancer Invest 17 (3): 223-30, 1999.
-
Paulino AC, Simon JH, Zhen W, et al.: Long-term effects in children treated with radiotherapy for head and neck rhabdomyosarcoma. Int J Radiat Oncol Biol Phys 48 (5): 1489-95, 2000.
-
Maciel JC, de Castro CG Jr, Brunetto AL, et al.: Oral health and dental anomalies in patients treated for leukemia in childhood and adolescence. Pediatr Blood Cancer 53 (3): 361-5, 2009.
-
Hsieh SG, Hibbert S, Shaw P, et al.: Association of cyclophosphamide use with dental developmental defects and salivary gland dysfunction in recipients of childhood antineoplastic therapy. Cancer 117 (10): 2219-27, 2011.
-
Dahllöf G: Oral and dental late effects after pediatric stem cell transplantation. Biol Blood Marrow Transplant 14 (1 Suppl 1): 81-3, 2008.
-
Hölttä P, Alaluusua S, Saarinen-Pihkala UM, et al.: Long-term adverse effects on dentition in children with poor-risk neuroblastoma treated with high-dose chemotherapy and autologous stem cell transplantation with or without total body irradiation. Bone Marrow Transplant 29 (2): 121-7, 2002.
-
Fromm M, Littman P, Raney RB, et al.: Late effects after treatment of twenty children with soft tissue sarcomas of the head and neck. Experience at a single institution with a review of the literature. Cancer 57 (10): 2070-6, 1986.
-
Thompson RF, Schneider RA, Albertini F, et al.: Dose to the developing dentition during therapeutic irradiation: organ at risk determination and clinical implications. Int J Radiat Oncol Biol Phys 86 (1): 108-13, 2013.
-
Maguire A, Craft AW, Evans RG, et al.: The long-term effects of treatment on the dental condition of children surviving malignant disease. Cancer 60 (10): 2570-5, 1987.
-
Alpaslan G, Alpaslan C, Gögen H, et al.: Disturbances in oral and dental structures in patients with pediatric lymphoma after chemotherapy: a preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87 (3): 317-21, 1999.
-
Kaste SC, Hopkins KP, Jones D, et al.: Dental abnormalities in children treated for acute lymphoblastic leukemia. Leukemia 11 (6): 792-6, 1997.
-
O'Sullivan EA, Duggal MS, Bailey CC: Changes in the oral health of children during treatment for acute lymphoblastic leukaemia. Int J Paediatr Dent 4 (1): 31-4, 1994.
-
Jensen SB, Pedersen AM, Vissink A, et al.: A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: prevalence, severity and impact on quality of life. Support Care Cancer 18 (8): 1039-60, 2010.
-
Jensen SB, Pedersen AM, Vissink A, et al.: A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: management strategies and economic impact. Support Care Cancer 18 (8): 1061-79, 2010.
-
Garming Legert K, Remberger M, Ringdèn O, et al.: Salivary secretion in children after fractionated or single-dose TBI. Bone Marrow Transplant 47 (3): 404-10, 2012.
-
Dahllöf G, Wondimu B, Barr-Agholme M, et al.: Xerostomia in children and adolescents after stem cell transplantation conditioned with total body irradiation or busulfan. Oral Oncol 47 (9): 915-9, 2011.
-
Garming-Legert K, Remberger M, Ringdén O, et al.: Long-term salivary function after conditioning with busulfan, fractionated or single-dose TBI. Oral Dis 17 (7): 670-6, 2011.
-
Raney RB, Asmar L, Vassilopoulou-Sellin R, et al.: Late complications of therapy in 213 children with localized, nonorbital soft-tissue sarcoma of the head and neck: A descriptive report from the Intergroup Rhabdomyosarcoma Studies (IRS)-II and - III. IRS Group of the Children's Cancer Group and the Pediatric Oncology Group. Med Pediatr Oncol 33 (4): 362-71, 1999.
-
Gevorgyan A, La Scala GC, Neligan PC, et al.: Radiation-induced craniofacial bone growth disturbances. J Craniofac Surg 18 (5): 1001-7, 2007.
-
Hong CH, Napeñas JJ, Hodgson BD, et al.: A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer 18 (8): 1007-21, 2010.
-
Yeazel MW, Gurney JG, Oeffinger KC, et al.: An examination of the dental utilization practices of adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Public Health Dent 64 (1): 50-4, 2004.
-
Goldsby R, Chen Y, Raber S, et al.: Survivors of childhood cancer have increased risk of gastrointestinal complications later in life. Gastroenterology 140 (5): 1464-71.e1, 2011.
-
Skou AS, Glosli H, Jahnukainen K, et al.: Renal, gastrointestinal, and hepatic late effects in survivors of childhood acute myeloid leukemia treated with chemotherapy only--a NOPHO-AML study. Pediatr Blood Cancer 61 (9): 1638-43, 2014.
-
Bölling T, Willich N, Ernst I: Late effects of abdominal irradiation in children: a review of the literature. Anticancer Res 30 (1): 227-31, 2010.
-
Churnratanakul S, Wirzba B, Lam T, et al.: Radiation and the small intestine. Future perspectives for preventive therapy. Dig Dis 8 (1): 45-60, 1990.
-
Sher ME, Bauer J: Radiation-induced enteropathy. Am J Gastroenterol 85 (2): 121-8, 1990.
-
Emami B, Lyman J, Brown A, et al.: Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21 (1): 109-22, 1991.
-
Donaldson SS, Jundt S, Ricour C, et al.: Radiation enteritis in children. A retrospective review, clinicopathologic correlation, and dietary management. Cancer 35 (4): 1167-78, 1975.
-
Heyn R, Raney RB Jr, Hays DM, et al.: Late effects of therapy in patients with paratesticular rhabdomyosarcoma. Intergroup Rhabdomyosarcoma Study Committee. J Clin Oncol 10 (4): 614-23, 1992.
-
Hughes LL, Baruzzi MJ, Ribeiro RC, et al.: Paratesticular rhabdomyosarcoma: delayed effects of multimodality therapy and implications for current management. Cancer 73 (2): 476-82, 1994.
-
Paulino AC, Wen BC, Brown CK, et al.: Late effects in children treated with radiation therapy for Wilms' tumor. Int J Radiat Oncol Biol Phys 46 (5): 1239-46, 2000.
-
Raney B Jr, Heyn R, Hays DM, et al.: Sequelae of treatment in 109 patients followed for 5 to 15 years after diagnosis of sarcoma of the bladder and prostate. A report from the Intergroup Rhabdomyosarcoma Study Committee. Cancer 71 (7): 2387-94, 1993.
-
Madenci AL, Fisher S, Diller LR, et al.: Intestinal Obstruction in Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study. J Clin Oncol 33 (26): 2893-900, 2015.
-
Mulder RL, van Dalen EC, Van den Hof M, et al.: Hepatic late adverse effects after antineoplastic treatment for childhood cancer. Cochrane Database Syst Rev (7): CD008205, 2011.
-
Mulder RL, Kremer LC, Koot BG, et al.: Surveillance of hepatic late adverse effects in a large cohort of long-term survivors of childhood cancer: prevalence and risk factors. Eur J Cancer 49 (1): 185-93, 2013.
-
Mahmoud H, Schell M, Pui CH: Cholelithiasis after treatment for childhood cancer. Cancer 67 (5): 1439-42, 1991.
-
Safford SD, Safford KM, Martin P, et al.: Management of cholelithiasis in pediatric patients who undergo bone marrow transplantation. J Pediatr Surg 36 (1): 86-90, 2001.
-
Sudour H, Mainard L, Baumann C, et al.: Focal nodular hyperplasia of the liver following hematopoietic SCT. Bone Marrow Transplant 43 (2): 127-32, 2009.
-
Lee MH, Yoo SY, Kim JH, et al.: Hypervascular hepatic nodules in childhood cancer survivors: clinical and imaging features. Clin Imaging 36 (4): 301-7, 2012 Jul-Aug.
-
Wanless IR: Micronodular transformation (nodular regenerative hyperplasia) of the liver: a report of 64 cases among 2,500 autopsies and a new classification of benign hepatocellular nodules. Hepatology 11 (5): 787-97, 1990.
-
Brisse H, Servois V, Bouche B, et al.: Hepatic regenerating nodules: a mimic of recurrent cancer in children. Pediatr Radiol 30 (6): 386-93, 2000.
-
Chu WC, Roebuck DJ: Nodular regenerative hyperplasia of the liver simulating metastases following treatment for bilateral Wilms tumor. Med Pediatr Oncol 41 (1): 85-7, 2003.
-
Halonen P, Mattila J, Ruuska T, et al.: Liver histology after current intensified therapy for childhood acute lymphoblastic leukemia: microvesicular fatty change and siderosis are the main findings. Med Pediatr Oncol 40 (3): 148-54, 2003.
-
Tomita Y, Ishiguro H, Yasuda Y, et al.: High incidence of fatty liver and insulin resistance in long-term adult survivors of childhood SCT. Bone Marrow Transplant 46 (3): 416-25, 2011.
-
Ruccione KS, Wood JC, Sposto R, et al.: Characterization of transfusion-derived iron deposition in childhood cancer survivors. Cancer Epidemiol Biomarkers Prev 23 (9): 1913-9, 2014.
-
Vag T, Kentouche K, Krumbein I, et al.: Noninvasive measurement of liver iron concentration at MRI in children with acute leukemia: initial results. Pediatr Radiol 41 (8): 980-4, 2011.
-
Broxson EH, Dole M, Wong R, et al.: Portal hypertension develops in a subset of children with standard risk acute lymphoblastic leukemia treated with oral 6-thioguanine during maintenance therapy. Pediatr Blood Cancer 44 (3): 226-31, 2005.
-
De Bruyne R, Portmann B, Samyn M, et al.: Chronic liver disease related to 6-thioguanine in children with acute lymphoblastic leukaemia. J Hepatol 44 (2): 407-10, 2006.
-
Rawat D, Gillett PM, Devadason D, et al.: Long-term follow-up of children with 6-thioguanine-related chronic hepatoxicity following treatment for acute lymphoblastic leukaemia. J Pediatr Gastroenterol Nutr 53 (5): 478-9, 2011.
-
Green DM, Norkool P, Breslow NE, et al.: Severe hepatic toxicity after treatment with vincristine and dactinomycin using single-dose or divided-dose schedules: a report from the National Wilms' Tumor Study. J Clin Oncol 8 (9): 1525-30, 1990.
-
Sulis ML, Bessmertny O, Granowetter L, et al.: Veno-occlusive disease in pediatric patients receiving actinomycin D and vincristine only for the treatment of rhabdomyosarcoma. J Pediatr Hematol Oncol 26 (12): 843-6, 2004.
-
McDonald GB: Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology 51 (4): 1450-60, 2010.
-
Dawson LA, Ten Haken RK: Partial volume tolerance of the liver to radiation. Semin Radiat Oncol 15 (4): 279-83, 2005.
-
Milano MT, Constine LS, Okunieff P: Normal tissue tolerance dose metrics for radiation therapy of major organs. Semin Radiat Oncol 17 (2): 131-40, 2007.
-
Pan CC, Kavanagh BD, Dawson LA, et al.: Radiation-associated liver injury. Int J Radiat Oncol Biol Phys 76 (3 Suppl): S94-100, 2010.
-
Bhanot P, Cushing B, Philippart A, et al.: Hepatic irradiation and adriamycin cardiotoxicity. J Pediatr 95 (4): 561-3, 1979.
-
Flentje M, Weirich A, Pötter R, et al.: Hepatotoxicity in irradiated nephroblastoma patients during postoperative treatment according to SIOP9/GPOH. Radiother Oncol 31 (3): 222-8, 1994.
-
Kun LE, Camitta BM: Hepatopathy following irradiation and adriamycin. Cancer 42 (1): 81-4, 1978.
-
Tefft M: Radiation related toxicities in National Wilms' Tumor Study Number 1. Int J Radiat Oncol Biol Phys 2 (5-6): 455-63, 1977 May-Jun.
-
Castellino S, Muir A, Shah A, et al.: Hepato-biliary late effects in survivors of childhood and adolescent cancer: a report from the Children's Oncology Group. Pediatr Blood Cancer 54 (5): 663-9, 2010.
-
Levitsky J, Sorrell MF: Hepatic complications of hematopoietic cell transplantation. Curr Gastroenterol Rep 9 (1): 60-5, 2007.
-
Pidala J, Chai X, Kurland BF, et al.: Analysis of gastrointestinal and hepatic chronic graft-versus-host [corrected] disease manifestations on major outcomes: a chronic graft-versus-host [corrected] disease consortium study. Biol Blood Marrow Transplant 19 (5): 784-91, 2013.
-
Tomás JF, Pinilla I, García-Buey ML, et al.: Long-term liver dysfunction after allogeneic bone marrow transplantation: clinical features and course in 61 patients. Bone Marrow Transplant 26 (6): 649-55, 2000.
-
Aricò M, Maggiore G, Silini E, et al.: Hepatitis C virus infection in children treated for acute lymphoblastic leukemia. Blood 84 (9): 2919-22, 1994.
-
Castellino S, Lensing S, Riely C, et al.: The epidemiology of chronic hepatitis C infection in survivors of childhood cancer: an update of the St Jude Children's Research Hospital hepatitis C seropositive cohort. Blood 103 (7): 2460-6, 2004.
-
Cesaro S, Petris MG, Rossetti F, et al.: Chronic hepatitis C virus infection after treatment for pediatric malignancy. Blood 90 (3): 1315-20, 1997.
-
Fink FM, Höcker-Schulz S, Mor W, et al.: Association of hepatitis C virus infection with chronic liver disease in paediatric cancer patients. Eur J Pediatr 152 (6): 490-2, 1993.
-
Locasciulli A, Testa M, Pontisso P, et al.: Hepatitis C virus genotypes and liver disease in patients undergoing allogeneic bone marrow transplantation. Bone Marrow Transplant 19 (3): 237-40, 1997.
-
Locasciulli A, Testa M, Pontisso P, et al.: Prevalence and natural history of hepatitis C infection in patients cured of childhood leukemia. Blood 90 (11): 4628-33, 1997.
-
Paul IM, Sanders J, Ruggiero F, et al.: Chronic hepatitis C virus infections in leukemia survivors: prevalence, viral load, and severity of liver disease. Blood 93 (11): 3672-7, 1999.
-
Lansdale M, Castellino S, Marina N, et al.: Knowledge of hepatitis C virus screening in long-term pediatric cancer survivors: a report from the Childhood Cancer Survivor Study. Cancer 116 (4): 974-82, 2010.
-
van Waas M, Neggers SJ, Raat H, et al.: Abdominal radiotherapy: a major determinant of metabolic syndrome in nephroblastoma and neuroblastoma survivors. PLoS One 7 (12): e52237, 2012.
-
Neville KA, Cohn RJ, Steinbeck KS, et al.: Hyperinsulinemia, impaired glucose tolerance, and diabetes mellitus in survivors of childhood cancer: prevalence and risk factors. J Clin Endocrinol Metab 91 (11): 4401-7, 2006.
-
Baker KS, Ness KK, Steinberger J, et al.: Diabetes, hypertension, and cardiovascular events in survivors of hematopoietic cell transplantation: a report from the bone marrow transplantation survivor study. Blood 109 (4): 1765-72, 2007.
-
de Vathaire F, El-Fayech C, Ben Ayed FF, et al.: Radiation dose to the pancreas and risk of diabetes mellitus in childhood cancer survivors: a retrospective cohort study. Lancet Oncol 13 (10): 1002-10, 2012.
-
van Nimwegen FA, Schaapveld M, Janus CP, et al.: Risk of diabetes mellitus in long-term survivors of Hodgkin lymphoma. J Clin Oncol 32 (29): 3257-63, 2014.
-
Meacham LR, Chow EJ, Ness KK, et al.: Cardiovascular risk factors in adult survivors of pediatric cancer--a report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev 19 (1): 170-81, 2010.
Late Effects of the Endocrine SystemEndocrine dysfunction is very common among childhood cancer survivors, especially those treated with surgery or radiation therapy that involves hormone-producing organs and those receiving alkylating agent chemotherapy.
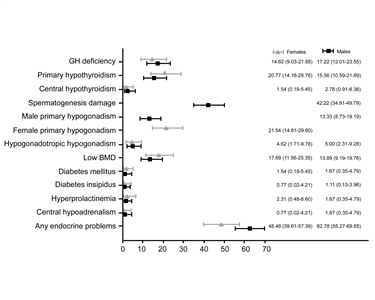
Figure 6. Prevalence of endocrine disorders at the last follow-up visit, by gender. Copyright © 2013, European Society of Endocrinology.
The prevalence of specific endocrine disorders varies by patient (e.g., age at treatment and sex) and treatment factors (e.g., radiation dose and treatment volume), and typically increases with longer time from radiation exposure (refer to Figure 6).[1,2,3] Endocrinologic late effects can be broadly categorized as those resulting from hypothalamic/pituitary injury or from peripheral glandular compromise.[4,5] The former are most common after treatment for central nervous system (CNS) tumors, where the prevalence was reported to be 24.8% in a nationwide cohort study of 718 survivors who lived longer than 2 years and all hypothalamic/pituitary axes were effected.[3] The following sections summarize research that characterizes the clinical features of survivors at risk of endocrine dysfunction that impacts pituitary, thyroid, adrenal, and gonadal function. Thyroid Gland Thyroid dysfunction is a common delayed effect of radiation therapy fields that include the thyroid gland incidental to treating Hodgkin lymphoma (HL), brain tumors, head and neck sarcomas, and acute lymphoblastic leukemia (ALL). There is considerable evidence linking radiation exposure to thyroid abnormalities, but the prevalence of specific conditions varies widely because studies are limited by cohort selection and participation bias, heterogeneity in radiation treatment approach, time since radiation exposure, and method of ascertainment (e.g., self-report vs. clinical or diagnostic imaging assessment). Thyroid abnormalities observed in excess in childhood cancer survivors include the following: - Primary hypothyroidism.
- Hyperthyroidism.
- Goiter.
- Nodules.
Hypothyroidism Of children treated with radiation therapy, most develop hypothyroidism within the first 2 to 5 years posttreatment, but new cases can occur later. Reports of thyroid dysfunction differ depending on the dose of radiation, the length of follow-up, and the biochemical criteria utilized to make the diagnosis.[6] The most frequently reported abnormalities include: - Elevated thyroid-stimulating hormone (TSH).
- Depressed thyroxine (T4).
- Elevated TSH and depressed T4.
Compensated hypothyroidism includes an elevated TSH with a normal T4 and is asymptomatic. The natural history is unclear, but most endocrinologists support treatment. Uncompensated hypothyroidism includes both an elevated TSH and a depressed T4. Thyroid hormone replacement is beneficial for correction of the metabolic abnormality, and has clinical benefits for cardiovascular, gastrointestinal, and neurocognitive function. An increased risk of hypothyroidism has been reported among childhood cancer survivors treated with head and neck radiation exposing the thyroid gland, especially among survivors of HL. Results from selected studies include the following: - The German Group of Paediatric Radiation Oncology reported on 1,086 patients treated at 62 centers, including 404 patients (median age, 10.9 years) who received radiation therapy to the thyroid and/or pituitary gland.[7] Follow-up information was available for 264 patients (60.9%; median follow-up, 40 months), with 60 patients (22.7%) showing pathologic values. The following was observed:
- In comparison to patients treated with prophylactic cranial irradiation (median dose, 12 Gy), patients treated with radiation doses of 15 Gy to 25 Gy to the thyroid gland had a hazard ratio (HR) of 3.072 (P = .002) for the development of pathologic thyroid blood values.
- Patients treated with more than 25 Gy of radiation to the thyroid gland had an HR of 3.769 (P = .009), and patients treated with craniospinal irradiation had an HR of 5.674 (P < .001).
- The cumulative incidence of thyroid hormone substitution therapy did not differ between defined subgroups.
- In a cohort of childhood HL survivors treated between 1970 and 1986, survivors were evaluated for thyroid disease by use of a self-report questionnaire in the Childhood Cancer Survivor Study (CCSS).[8] Among 1,791 survivors, 34% reported that they had been diagnosed with at least one thyroid abnormality. For hypothyroidism, there was a clear dose response (refer to Figure 7), with a 20-year risk of:
- 20% for those who received less than 35 Gy of radiation to the thyroid gland.
- 30% for those who received 35 Gy to 44.9 Gy of radiation to the thyroid gland.
- 50% for those who received more than 45 Gy of radiation to the thyroid gland.
Compared to a sibling control group, the relative risk (RR) was 17.1 for hypothyroidism; 8.0 for hyperthyroidism; and 27.0 for thyroid nodules. Elapsed time since diagnosis was a risk factor for both hypothyroidism and hyperthyroidism, with the risk increasing in the first 3 to 5 years postdiagnosis. For nodules, the risk increased beginning at 10 years postdiagnosis. Females were at increased risk for hypothyroidism and thyroid nodules.
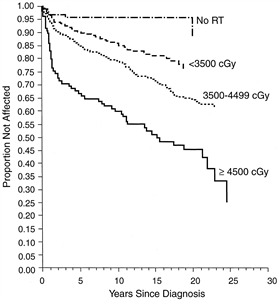
Figure 7. Probability of developing hypothyroidism according to radiation dose in 5-year survivors of childhood cancer. Data from the Childhood Cancer Survivor Study. Sklar C, Whitton J, Mertens A, Stovall M, Green D, Marina N, Greffe B, Wolden S, Robison L: Abnormalities of the Thyroid in Survivors of Hodgkin's Disease: Data from the Childhood Cancer Survivor Study. The Journal of Clinical Endocrinology and Metabolism 85 (9): 3227-3232, September 1, 2000. Copyright 2000, The Endocrine Society.
- In a more recent report from the CCSS that compared self-reported data from 14,290 survivors with data from 4,031 sibling controls, the RR was 3.8 for hypothyroidism and 2.5 for hyperthyroidism; the RR for both remained significantly higher in survivors when compared with controls even in the absence of radiation therapy to the thyroid or pituitary.[2] These results indicate the need for continued and individualized long-term monitoring strategies in childhood cancer survivors.
Thyroid nodules Any radiation field that includes the thyroid is associated with an excess risk of thyroid neoplasms, which may be benign (usually adenomas) or malignant (most often differentiated papillary carcinoma).[2,8,9,10,11,12] The clinical manifestation of thyroid neoplasia among childhood cancer survivors ranges from asymptomatic, small, solitary nodules to large, intrathoracic goiters that compress adjacent structures. CCSS investigators performed a nested case-control study to evaluate the magnitude of risk for thyroid cancer over the therapeutic radiation dose range of pediatric cancers. The risk of thyroid cancer increased with radiation doses up to 20 Gy to 29 Gy (odds ratio [OR], 9.8; 95% confidence interval [CI], 3.2-34.8), but declined at doses higher than 30 Gy, consistent with a cell-killing effect.[12] The following factors are linked to an increased risk of thyroid nodule development: - Time from diagnosis, female gender, and radiation dose. In a study of HL survivors, CCSS investigators identified time from diagnosis, female gender, and radiation dose of 25 Gy or higher as significant risk factors for thyroid nodule development.[8] Based on a cohort of 3,254 2-year childhood cancer survivors treated before 1986 and monitored for 25 years, the risk of thyroid adenoma increased with the size of the radiation dose to the thyroid during childhood cancer treatment and plateaued at doses exceeding 10 Gy.[10]
- Age at time of radiation therapy. Based on the same cohort of 3,254 2-year childhood cancer survivors, the risk of thyroid adenoma per unit of radiation dose to the thyroid was higher if radiation therapy had been delivered before age 5 years; the risk was also higher in individuals who were younger than 40 years at the time of the study.[10] Younger age at radiation therapy has also been linked to an excess risk of thyroid carcinoma.[9,10,11,12]
- Exposure to iodine I 131 metaiodobenzylguanidine (131 I-mIBG). During childhood and adolescence, there is an increased incidence of developing thyroid nodules, and potentially thyroid cancer, for patients exposed to 131 I-mIBG. Children who have been treated with 131 I-mIBG should undergo lifelong monitoring, not only for thyroid function but also for the development of thyroid nodules and thyroid cancer.[13]
- Chemotherapy. Whereas the risk of thyroid cancer is known to be increased by exposure to radiation therapy and 131 I-mIBG, an increased risk of thyroid nodules and cancer has also been observed in association with chemotherapy, independent of radiation exposure.[2,9,10]
In a pooled study of two cohorts of 16,757 survivors that included 187 patients with secondary thyroid cancer, treatments with alkylating agents, anthracyclines, or bleomycin were associated with a significantly increased risk of thyroid cancer in individuals not exposed to radiation therapy.[14] In the CCSS, the RR of developing thyroid cancer was 2.5 (P < .01) in survivors not treated with thyroid radiation when compared with sibling controls.[2] Defining the precise role of exposure to chemotherapy and developing risk prediction models for thyroid cancer in childhood cancer survivors on the basis of demographic and treatment-related risk factors are areas of active research.[15]
Several investigations have demonstrated the superiority of ultrasound to clinical exam for detecting thyroid nodules and thyroid cancers and characterized ultrasonographic features of nodules that are more likely to be malignant.[16,17,18] However, primary screening for thyroid neoplasia (beyond physical exam with thyroid palpation) remains controversial because of the lack of data indicating a survival benefit and quality-of-life benefit associated with early detection and intervention. In fact, because these lesions tend to be indolent, are rarely life-threatening, and may clinically manifest many years after exposure to radiation, there are significant concerns regarding the costs and harms of overscreening.[19] Expert panels have refrained from specifically endorsing or discouraging the use of ultrasound as a screening tool for thyroid cancer and this continues to be an active area of investigation.[20] (Refer to the Subsequent Neoplasms section of this summary for information about subsequent thyroid cancers.) Posttransplant thyroid dysfunction Survivors of pediatric hematopoietic stem cell transplantation (HSCT) are at increased risk of thyroid dysfunction, with the risk being much lower (15%-16%) after fractionated total-body irradiation (TBI), as opposed to single-dose TBI (46%-48%). Non-TBI-containing regimens historically were not associated with an increased risk. However, in a report from the Fred Hutchinson Cancer Research Center, the increased risk of thyroid dysfunction did not differ between children receiving a TBI-based or busulfan-based regimen (P = .48).[21] Other high-dose therapies have not been studied. Table 7. Thyroid Late Effectsa| Predisposing Therapy | Endocrine/Metabolic Effects | Health Screening |
|---|
| mIBG = metaiodobenzylguanidine; T4 = thyroxine; TSH = thyroid-stimulating hormone. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Radiation impacting thyroid gland; thyroidectomy | Primary hypothyroidism | TSH level | | Radiation impacting thyroid gland | Hyperthyroidism | Free T4 level | | TSH level | | Radiation impacting thyroid gland, including mIBG | Thyroid nodules | Thyroid exam | | Thyroid ultrasound | TSH deficiency (central hypothyroidism) is discussed with late effects that affect the pituitary gland. Pituitary Gland Survivors of childhood cancer are at risk of developing a spectrum of neuroendocrine abnormalities, primarily because of the effect of radiation therapy on the hypothalamus. In addition, tumor development or surgical resection close to the hypothalamus and/or pituitary gland may induce direct anatomical damage to these structures and result in hypothalamic/pituitary dysfunction. Essentially all of the hypothalamic-pituitary axes are at risk.[4,22,23,24] Although the quality of the literature regarding pituitary endocrinopathy among childhood cancer survivors is often limited by retrospective data collection, small sample size, cohort selection and participation bias, heterogeneity in treatment approach, time since treatment, and method of ascertainment, the evidence linking this outcome with radiation therapy, surgery, and tumor infiltration is quite compelling because affected individuals typically present with metabolic and developmental abnormalities early in follow-up. Central diabetes insipidus Central diabetes insipidus may herald the diagnosis of craniopharyngioma, suprasellar germ cell tumor, or Langerhans cell histiocytosis.[25,26,27] In these conditions, diabetes insipidus may occur as an isolated pituitary deficiency, although additional pituitary hormone deficiencies may develop with tumor progression. More commonly, however, diabetes insipidus occurs in the context of panhypopituitarism caused by the presence of a tumor in close proximity to the sellar region or as a consequence of surgical procedures undertaken for local tumor control. Central diabetes insipidus has not been reported as a late effect of cranial irradiation in childhood cancer survivors. Anterior pituitary hormone deficiency Deficiencies of anterior pituitary hormones and major hypothalamic regulatory factors are common late effects among survivors treated with cranial irradiation. In a study of 1,713 adult survivors of childhood cancers and brain tumors (median age, 32 years) monitored in a single institution (median follow-up, 25 years), the prevalence of hypothalamic-pituitary axis disorders was 56.4% in individuals exposed to cranial radiation therapy at doses of 18 Gy or higher.[24] Among 748 childhood cancer survivors treated with cranial irradiation and observed for a mean of 27.3 years, the estimated point prevalence for anterior pituitary hormone deficiency was 46.5% for growth hormone deficiency (GHD), 10.8% for luteinizing/follicle stimulating hormone deficiency, 7.5% for thyroid-stimulating hormone deficiency, and 4% for adrenocorticotropin deficiency; the cumulative incidence increased with follow-up.[5] The six anterior pituitary hormones and their major hypothalamic regulatory factors are outlined in Table 8. Table 8. Anterior Pituitary Hormones and Major Hypothalamic Regulatory Factors| Pituitary Hormone | Hypothalamic Factor | Hypothalamic Regulation of the Pituitary Hormone |
|---|
| (-) = inhibitory; (+) = stimulatory. | | Growth hormone (GH) | Growth hormone-releasing hormone | + | | Somatostatin | - | | Prolactin | Dopamine | - | | Luteinizing hormone (LH) | Gonadotropin-releasing hormone | + | | Follicle-stimulating hormone (FSH) | Gonadotropin-releasing hormone | + | | Thyroid-stimulating hormone (TSH) | Thyroid-releasing hormone | + | | Somatostatin | - | | Adrenocorticotropin (ACTH) | Corticotropin-releasing hormone | + | | Vasopressin | + | Growth hormone deficiency (GHD) GHD is the earliest hormonal deficiency associated with cranial radiation therapy in childhood cancer survivors. The risk increases with radiation dose and time since treatment. GHD is sensitive to low doses of radiation. Other hormone deficiencies require higher doses, and their time to onset is much longer than for GHD.[28] The prevalence in pooled analysis was found to be approximately 35.6%.[29] GHD is commonly observed in these long-term survivors because of radiation doses used in the treatment of childhood brain tumors. Approximately 60% to 80% of irradiated pediatric brain tumor patients who received doses higher than 30 Gy will have impaired serum growth hormone (GH) response to provocative stimulation, usually within 5 years of treatment. The dose-response relationship has a threshold of 18 Gy to 20 Gy; the higher the radiation dose, the earlier that GHD will occur after treatment. - A study of conformal radiation therapy (CRT) in children with CNS tumors indicates that GH insufficiency can usually be demonstrated within 12 months of radiation therapy, depending on hypothalamic dose-volume effects.[30]
- In a report featuring data from 118 patients with localized brain tumors who were treated with radiation therapy, peak GH was modeled as an exponential function of time after CRT and mean radiation dose to the hypothalamus. The average patient was predicted to develop GHD with the following combinations of time after CRT and mean dose to the hypothalamus: 12 months and more than 60 Gy; 36 months and 25 Gy to 30 Gy; and 60 months and 15 Gy to 20 Gy. A cumulative dose of 16.1 Gy to the hypothalamus would be considered the mean radiation dose required to achieve a 50% risk of GHD at 5 years (TD50/5) (refer to Figure 8).[31]
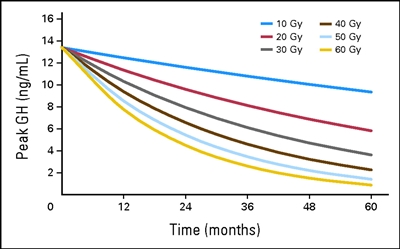
Figure 8. Peak growth hormone (GH) according to hypothalamic mean dose and time after start of radiation. According to equation 2, peak GH = exp{2.5947 + time × [0.0019 − (0.00079 × mean dose)]}. Thomas E. Merchant, Susan R. Rose, Christina Bosley, Shengjie Wu, Xiaoping Xiong, and Robert H. Lustig, Growth Hormone Secretion After Conformal Radiation Therapy in Pediatric Patients With Localized Brain Tumors, Journal of Clinical Oncology, volume 29, issue 36, pages 4776-4780. Reprinted with permission. © (2011) American Society of Clinical Oncology. All rights reserved.
Children treated with CNS-directed therapy for leukemia are also at increased risk of GHD. Results from selected studies of childhood ALL survivors are as follows: - One study evaluated 127 patients with ALL treated with 24 Gy, 18 Gy, or no cranial radiation therapy. The change in height, compared with population norms expressed as the standard deviation score (SDS), was significant for all three groups, with a dose response of -0.49 ± 0.14 for the group that did not receive radiation therapy, -0.65 ± 0.15 for the group that received 18 Gy of radiation therapy, and -1.38 ± 0.16 for the group that received 24 Gy of radiation therapy.[32]
- Another study found similar results in 118 ALL survivors treated with 24 Gy of cranial radiation, in which 74% had SDS of -1 or higher and the remainder had scores of -2 or higher.[33]
- Survivors of childhood ALL who are treated with chemotherapy alone are also at increased risk for adult short stature, although the risk is highest for those treated with cranial and craniospinal radiation therapy at a young age.[34] In this cross-sectional study, attained adult height was determined for 2,434 ALL survivors participating in the CCSS.
- All survivor treatment exposure groups (chemotherapy alone and chemotherapy with cranial or craniospinal radiation therapy) had decreased adult height and an increased risk of adult short stature (height SDS < -2), compared with siblings (P < .001).
- Compared with siblings, the risk of short stature for survivors treated with chemotherapy alone was elevated (OR, 3.4; 95% CI, 1.9-6.0).
- Among survivors, significant risk factors for short stature included diagnosis of ALL before puberty, higher-dose cranial radiation therapy (≥20 Gy vs. <20 Gy), any radiation therapy to the spine, and female gender.
- The impact of chemotherapy alone on growth in 67 survivors treated with contemporary regimens for ALL was statistically significant at -0.59 SD. The loss of growth potential did not correlate with GH status in this study, further highlighting the participation of other factors in the growth impairments observed in this population.[35]
Children who undergo HSCT with TBI have a significant risk of both GHD and the direct effects of radiation on skeletal development. The risk is increased with single-dose TBI as opposed to fractionated TBI, pretransplant cranial irradiation, female gender, and posttreatment complications such as graft-versus-host disease (GVHD).[36,37,38] Regimens containing busulfan and cyclophosphamide appear to increase risk in some studies,[38,39] but not others.[40] Hyperfractionation of the TBI dose markedly reduces risk in patients who have not undergone pretransplant cranial irradiation for CNS leukemia prophylaxis or therapy.[41] The late effects that occur after HSCT have been studied and reviewed by the Late Effect Working Party of the European Group for Blood and Marrow Transplantation. Among 181 patients with aplastic anemia, leukemias, and lymphomas who underwent HSCT before puberty, the following results were observed:[42,43] - An overall decrease in final height-SDS value was found, compared with height at transplant and genetic height. The mean loss of height is estimated to be approximately 1 height-SDS (6 cm), compared with the mean height at time of HSCT and mean genetic height.
- The type of transplantation, GVHD, and GH or steroid treatment did not influence final height.
- TBI (single-dose radiation therapy more than fractionated-dose radiation therapy), male gender, and young age at transplant were found to be major factors for long-term height loss. Most patients (140 of 181) reached adult height within the normal range of the general population.
GHD replacement therapy provides the benefit of optimizing height outcomes among children who have not reached skeletal maturity. Treatment with recombinant GH (rGH) replacement therapy is generally delayed until 12 months after successful completion of cancer or brain tumor treatments and after a multidisciplinary discussion involving the prescribing pediatric endocrinologist, the primary oncologist, and other providers selected by the patient or family.[44] Safety concerns pertaining to the use of rGH in childhood cancer survivors have primarily been related to the mitogenic potential of the GH stimulating tumor growth in a population with an increased risk of second neoplasms.[45] Most studies that report these outcomes, however, are limited by selection bias and small sample size. The following study results have been reported in survivors who did or did not receive treatment with GH: - One study evaluated 361 GH-treated cancer survivors enrolled in the CCSS and compared risk of recurrence, risk of subsequent neoplasm, and risk of death among survivors who did and did not receive treatment with GH.[46]
- The RR of disease recurrence was 0.83 (95% CI, 0.37-1.86) for GH-treated survivors. GH-treated subjects were diagnosed with 15 subsequent neoplasms, all solid tumors, for an overall RR of 3.21 (95% CI, 1.88-5.46), mainly because of a small excess number of subsequent neoplasms observed in survivors of acute leukemia.[46] With prolonged follow-up, the elevation of subsequent cancer risk resulting from GH diminished.[47]
- Compared with survivors not treated with GH, those who were treated had a twofold excess risk of developing a subsequent neoplasm (RR, 2.15; 95% CI, 1.33-3.47; P < .002); meningiomas were the most commonly observed neoplasms (9 of 20 tumors).
- A review of existing data suggests that treatment with GH is not associated with an increased risk of CNS tumor progression or recurrence, or new or recurrent leukemia.[48]
- A recent study from the CCSS reported specifically on the risk of subsequent CNS neoplasms after a longer period of follow-up. The adjusted rate ratio of meningioma and gliomas in GH-treated survivors of CNS tumors was 1.0 (95% CI, 0.6-1.8; P = .94) when compared with CNS tumor survivors who were not treated with GH, thus indicating negligible differences between the two groups for this particular risk.[49]
In general, the data addressing subsequent malignancies should be interpreted with caution given the small number of events.[44,45,46] Disorders of luteinizing hormone (LH) and follicle-stimulating hormone (FSH): Central precocious puberty and LH/FSH deficiency Pubertal development can be adversely affected by cranial radiation therapy. Doses higher than 18 Gy can result in central precocious puberty, while doses higher than 30 Gy to 40 Gy may result in LH and FSH deficiency.[50] Central precocious puberty Central precocious puberty is defined by the onset of pubertal development before age 8 years in girls and 9 years in boys as a result of the premature activation of the hypothalamic-pituitary-gonadal axis. Aside from the adjustment and psychosocial challenges associated with early pubertal development, precocious puberty can lead to the rapid closure of the skeletal growth plates and short stature. This deleterious effect can be further potentiated by GHD.[51,52] The increased growth velocity induced by pubertal development can mask concurrent GHD with seemingly normal growth velocity; this occurrence may mislead care providers. It is also important to note that the assessment of puberty cannot be performed using testicular volume measurements in boys exposed to chemotherapy or direct radiation to the testes, given the toxic effect of these treatments on germ cells and repercussions on gonadal size. The staging of puberty in males within this population relies on the presence of other signs of virilization, such as the presence of pubic hair and the measurement of plasma testosterone levels.[51] Children who have tumors that grow near the hypothalamus/pituitary or optic pathways (including those with neurofibromatosis type 1) have the highest risk of developing central precocious puberty.[52,53] Hydrocephalus also seems to increase the risk of this complication.[53] Central precocious puberty has been reported in some children receiving cranial irradiation in doses of 18 Gy or higher.[52,54,55] The impact of central precocious puberty on linear growth can be ascertained by assessing the degree of skeletal maturation (or bone age) using an x-ray of the left hand.[56] When appropriate, delaying the progression of puberty relies on the use of various gonadotropin-releasing hormone agonist preparations, an approach that has been shown to improve growth prospects-especially when other pituitary abnormalities, including GHD, are concurrently treated.[57] LH/FSH deficiency LH/FSH deficiency (also referred to as hypogonadotropic hypogonadism) can manifest through pubertal delay, arrested puberty, or symptoms of decreased sex hormone production, depending on age and pubertal status at the time of diagnosis. The risk of LH/FSH deficiency is highest among patients treated with cranial radiation at doses greater than or equal to 30 Gy; LH/FSH deficiency following the exposure to lower doses can occur at delayed time points.[5] With higher doses of cranial radiation therapy (>35 Gy), deficiencies in LH/FSH can be seen, with a cumulative incidence of 10% to 20% at 5 to 10 years posttreatment.[58,59] The treatment of LH/FSH deficiency relies on sex-hormone replacement therapy adjusted to age and pubertal status. TSH deficiency TSH deficiency (also referred to as central hypothyroidism) in survivors of childhood cancer can have profound clinical consequences and be underappreciated. Symptoms of central hypothyroidism (e.g., asthenia, edema, drowsiness, and skin dryness) may have a gradual onset and go unrecognized until thyroid replacement therapy is initiated. In addition to delayed puberty and slow growth, hypothyroidism may cause fatigue, dry skin, constipation, increased sleep requirement, and cold intolerance. Individuals with TSH deficiency have low plasma free T4 levels and either low or inappropriately normal TSH levels. The risk of TSH deficiency is highest among patients treated with cranial radiation at doses greater than or equal to 30 Gy; TSH deficiency following the exposure to lower doses can occur at delayed time points.[5] Radiation dose to the hypothalamus in excess of 42 Gy is associated with an increased risk of developing TSH deficiency (44% ± 19% for dose of ≥42 Gy and 11% ± 8% for dose of <42 Gy).[60] It occurs in as many as 65% of survivors of brain tumors, 43% of survivors of childhood nasopharyngeal tumors, 35% of bone marrow transplant recipients, and 10% to 15% of leukemia survivors.[61,62] Mixed primary and central hypothyroidism can also occur and reflects separate injuries to the thyroid gland and the hypothalamus (e.g., radiation injury to both structures). TSH values may be elevated and, in addition, the secretory dynamics of TSH are abnormal, with a blunted or absent TSH surge or a delayed peak response to TSH-releasing hormone (TRH).[63] In a study of 208 childhood cancer survivors referred for evaluation of possible hypothyroidism or hypopituitarism, mixed hypothyroidism was present in 15 patients (7%).[63] Among patients who received TBI (fractionated total doses of 12-14.4 Gy) or craniospinal radiation therapy (fractionated total cranial doses higher than 30 Gy), 15% had mixed hypothyroidism. In one study of 32 children treated for medulloblastoma, 56% developed hypothyroidism, including 38% with primary hypothyroidism and 19% with central hypothyroidism.[64] Thyroid hormone replacement therapy using levothyroxine represents the mainstay of treatment of TSH deficiency. The dose of levothyroxine needs to be adjusted solely using plasma free T4 levels; the levels of TSH are expected to remain low during therapy, given the central nature of this deficiency. Adrenal-corticotropin (ACTH) deficiency ACTH deficiency is less common than other neuroendocrine deficits but should be suspected in patients who have a history of brain tumor (regardless of therapy modality), cranial radiation therapy, GHD, or central hypothyroidism.[28,60,65,66,67] Although uncommon, ACTH deficiency can occur in patients treated with intracranial radiation doses of less than 24 Gy and has been reported to occur in fewer than 3% of patients after chemotherapy alone.[67] The diagnosis should be suspected when low plasma levels of morning cortisol are measured (a screening cortisol level collected at 8 a.m. that is 10 µg/dL or more is reassuring for ACTH sufficiency, whereas a value of 5 µg/dL or lower is suspicious for insufficiency). Confirmation is necessary using dynamic testing such as the low-dose ACTH stimulation test.[66] Because of the substantial risk of central adrenal insufficiency among survivors treated with cranial radiation doses exceeding 30 Gy to the hypothalamic-pituitary axis, endocrine monitoring with periodic dynamic testing as clinically indicated is recommended for this high-risk group. Patients with partial ACTH deficiency may have only subtle symptoms unless they become ill. Illness can disrupt these patients' usual homeostasis and cause a more severe, prolonged, or complicated course than expected. As in complete ACTH deficiency, incomplete or unrecognized ACTH deficiency can be life-threatening during concurrent illness. The treatment of ACTH deficiency relies on replacement with hydrocortisone, including stress dosing in situations of illness to adjust to the body's physiologically increased need for glucocorticoids. Hyperprolactinemia Hyperprolactinemia has been described in patients who received radiation therapy to the hypothalamus in doses higher than 50 Gy or who underwent surgery that disrupted the integrity of the pituitary stalk. Primary hypothyroidism may lead to hyperprolactinemia as a result of hyperplasia of thyrotrophs and lactotrophs, presumably due to TRH hypersecretion. The prolactin response to TRH is usually exaggerated in these patients.[28,68] In general, hyperprolactinemia may result in delayed puberty, galactorrhea, menstrual irregularities, loss of libido, hot flashes, infertility, and osteopenia. However, hyperprolactinemia resulting from cranial radiation therapy is rarely symptomatic and, given its frequent associations with hypogonadism (both central and primary), rarely requires treatment. Table 9. Pituitary Gland Late Effectsa| Predisposing Therapy | Endocrine/Metabolic Effects | Health Screening |
|---|
| BMI = body mass index; FSH = follicle-stimulating hormone; LH = luteinizing hormone; T4 = thyroxine; TSH = thyroid-stimulating hormone. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | b Testicular volume measurements are not reliable in the assessment of pubertal development in boys exposed to chemotherapy or direct radiation to the testes. | | c Appropriate only at diagnosis. TSH levels are not useful for follow-up during replacement therapy. | | Tumor or surgery affecting hypothalamus/pituitary. Radiation impacting hypothalamic-pituitary axis. | Growth hormone deficiency | Assessment of nutritional status | | Height, weight, BMI, Tanner stageb | | Tumor or surgery affecting hypothalamus/pituitary or optic pathways; hydrocephalus. Radiation impacting hypothalamic-pituitary axis. | Precocious puberty | Height, weight, BMI, Tanner stageb | | FSH, LH, estradiol, or testosterone levels | | Tumor or surgery affecting hypothalamus/pituitary. Radiation impacting hypothalamic-pituitary axis. | Gonadotropin deficiency | History: puberty, sexual function | | Exam: Tanner stageb | | FSH, LH, estradiol or testosterone levels | | Tumor or surgery affecting hypothalamus/pituitary. Radiation impacting hypothalamic-pituitary axis. | Central adrenal insufficiency | History: failure to thrive, anorexia, episodic dehydration, hypoglycemia, lethargy, unexplained hypotension | | Endocrine consultation for those with radiation dose ≥30 Gy | | Radiation impacting hypothalamic-pituitary axis. | Hyperprolactinemia | History/exam: galactorrhea | | Prolactin level | | Radiation impacting hypothalamic-pituitary axis. | Overweight/obesity | Height, weight, BMI | | Blood pressure | | Components of metabolic syndrome (abdominal obesity, hypertension, dyslipidemia, impaired glucose metabolism) | Fasting blood glucose level and lipid profile | | Tumor or surgery affecting hypothalamus/pituitary. Radiation impacting hypothalamic-pituitary axis. | Central hypothyroidism | TSHc free thyroxine (free T4) level | Testis and Ovary Testicular and ovarian hormonal functions are discussed in the Late Effects of the Reproductive System section of this summary. Metabolic Syndrome An increased risk of metabolic syndrome or its components has been observed among cancer survivors. The evidence for this outcome ranges from clinically manifested conditions that are self-reported by survivors to retrospectively assessed data in medical records and hospital registries to systematic clinical evaluations of clinically well-characterized cohorts. Studies have been limited by cohort selection and participation bias, heterogeneity in treatment approach, time since treatment, and method of ascertainment. Despite these limitations, compelling evidence indicates that metabolic syndrome is highly associated with cardiovascular events and mortality. Definitions of metabolic syndrome are evolving but generally include a combination of central (abdominal) obesity with at least two or more of the following features: - Hypertension.
- Atherogenic dyslipidemia (elevated triglycerides, reduced high-density lipoprotein [HDL] cholesterol).
- Abnormal glucose metabolism (fasting hyperglycemia, hyperinsulinism, insulin resistance, diabetes mellitus type 2).[69]
Long-term survivors of ALL, especially those treated with cranial radiation therapy, may have a higher prevalence of some potentially modifiable risk factors for cardiovascular disease such as impaired glucose tolerance or overt diabetes mellitus, dyslipidemia, hypertension, and obesity.[70,71,72,73,74,75,76] The contribution of modifiable risk factors associated with metabolic syndrome to the risk of major cardiac events suggests that survivors are good candidates for targeted screening and lifestyle counseling regarding risk-reduction measures.[77] Several studies have provided support for the potential benefits of lifestyle modifications in reducing cardiovascular disease risk. - Survivors participating in the St. Jude Lifetime Cohort Study who were adherent to a heart-healthy lifestyle had a lower risk of metabolic syndrome. Females (RR, 2.4; 95% CI, 1.7-3.3) and males (RR, 2.2; 95% CI, 1.6-3.0) in the cohort who did not follow recommended dietary and physical activity guidelines had a more than twofold excess risk of having clinical features of the metabolic syndrome.[78]
- In a CCSS investigation evaluating the impact of exercise on cardiovascular disease risk among survivors of HL, vigorous exercise was associated with a lower risk of cardiovascular events in a dose-dependent manner, independent of cardiovascular risk profile and treatment. Survivors who were adherent to national vigorous-intensity exercise guidelines had a 51% reduction in the risk of any cardiovascular event compared with those not meeting the guidelines.[79]
Results of selected studies describing the metabolic syndrome in childhood cancer cohorts include the following: - In a study of 784 long-term childhood ALL survivors (median age, 31.7 years; median follow-up, 26.1 years), the prevalence of metabolic syndrome was 33.6%, which was significantly higher than that in a cohort of age-, sex-, and race-matched controls (N = 777) from the National Health and Nutrition Examination Survey (RR, 1.43; 95% CI, 1.22-1.69). Risk factors associated with metabolic syndrome in this study included older age and past exposures to cranial radiation therapy. Components of metabolic syndrome with significantly higher prevalence in ALL survivors than in controls included obesity, insulin resistance, hypertension, and decreased HDL levels.[75]
- In a European cohort of 184 adult survivors of childhood leukemia (81.5% had ALL; median age, 21.2 years; median follow-up, 15.4 years), the prevalence of metabolic syndrome was 9.2%. In this study, exposure to TBI was found to be significantly associated with metabolic syndrome, with significant associations between TBI and hypertriglyceridemia, and low HDL and impaired fasting glucose.[76]
Abdominal irradiation is an additional risk factor for metabolic syndrome. Survivors of developmental or embryonal tumors treated with abdominal irradiation are also at an increased risk of developing components of metabolic syndrome. In a prospective study of 164 long-term survivors (median follow-up, 26 years), nephroblastoma (OR, 5.2) and neuroblastoma (OR, 6.5) survivors had more components of metabolic syndrome than did controls. Compared with nonirradiated survivors, survivors treated with abdominal irradiation had higher blood pressure, triglycerides, low-density lipoprotein (LDL) cholesterol, and total fat percentage, which were assessed by dual-energy x-ray absorptiometry.[80] Abnormal glucose metabolism Abdominal radiation therapy and TBI are increasingly recognized as independent risk factors for diabetes mellitus in childhood cancer survivors.[2,71,76,80,81,82,83,84,85] - A single-center cohort study of 532 long-term (median follow-up, 17.9 years) adult (median age, 25.6 years) survivors observed that treatment but not genetic variation was strongly associated with the occurrence of the components of metabolic syndrome. Metabolic syndrome was more frequent in cranially (23.3%, P = .002) and abdominally (23.4%, P = .009) irradiated survivors than in nonirradiated survivors (10.0%).[83]
- In a cross-sectional study evaluating cardiovascular risk factors and insulin resistance in a clinically heterogeneous cohort of 319 childhood cancer survivors 5 or more years since diagnosis and 208 sibling controls, insulin resistance was significantly higher in survivors treated with cisplatin plus cranial irradiation (92% brain tumors) and in those who received steroids but no cisplatin (most leukemia survivors), compared with siblings.[86] Insulin resistance did not differ between survivors treated with surgery alone and siblings. Among survivors, analysis of individual chemotherapy agents failed to find associations with cardiovascular risk factors or insulin resistance. However, compared with siblings, nearly all chemotherapeutic agents, when examined individually, seemed to be associated with a high cardiovascular risk profile, characterized by lower total lean body mass, higher percentage fat mass, and insulin resistance.
- In a European multicenter cohort of 2,520 childhood cancer survivors (median follow-up, 28 years), significant associations were found between diabetes mellitus and increasing doses of radiation therapy to the tail of the pancreas. These data support the contribution of radiation-induced islet cell injury to impairments of glucose homeostasis in this population.[84]
- In a report from the CCSS that compared 8,599 childhood cancer survivors to 2,936 randomly selected sibling controls, and after adjustment for age, body mass index (BMI), and several demographic factors, the risk of diabetes mellitus was 1.8 times higher in survivors (95% CI, 1.3-2.5; P < .001). Significant associations were found between diabetes mellitus and young age at diagnosis (0-4 years), the use of alkylating agents and abdominal radiation therapy or TBI. Also, survivors were significantly more likely to be receiving medication for hypertension, dyslipidemia, and/or diabetes mellitus than were sibling controls.[87]
Table 10. Metabolic Syndrome Late Effectsa| Predisposing Therapy | Potential Late Effects | Health Screening |
|---|
| BMI = body mass index. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Abdominal irradiation. Total-body irradiation. | Components of metabolic syndrome (abdominal obesity, hypertension, dyslipidemia, impaired glucose metabolism) | Height, weight, BMI, blood pressure | | Labs: fasting glucose and lipids | Body Composition: Underweight, Overweight, and Obesity Childhood cancer survivors are at risk of experiencing abnormal body composition, which includes being underweight (BMI, <18.5), overweight (BMI, >25.0 to BMI, <30.0), or obese (BMI, ≥30.0). BMI at diagnosis has been identified as a significant predictor of being underweight or overweight at follow-up, suggesting that genetic or environmental factors contribute to the development or persistence of abnormal body composition.[88,89] CCSS investigators identified treatment-related risk factors for being underweight, including TBI (females) or abdominal irradiation (males), use of alkylating agents, and use of anthracyclines.[89] Among a cohort of 893 Dutch childhood cancer survivors monitored for a median of almost 15 years, being underweight was linked to a high prevalence of moderate to extreme adverse health statuses and reports of a major medical condition.[88] To date, cancer patients with an increased incidence of being overweight and obese are primarily ALL [88,90,91,92,93,94,95,96] and CNS tumor [4,22] survivors who were treated with cranial radiation therapy.[89,97] In addition, craniopharyngioma survivors have a substantially increased risk of extreme obesity because of the tumor location and the hypothalamic damage resulting from surgical resection.[98,99,100,101,102,103] In addition to treatment factors, lifestyle factors and medication use can also contribute to the risk of obesity. CCSS investigators reported the following independent risk factors for obesity in childhood cancer survivors:[104] - Cancer diagnosed at ages 5 to 9 years (RR, 1.12; 95% CI, 1.01-1.24).
- Abnormal physical functioning (RR, 1.19; 95% CI, 1.06-1.33).
- Hypothalamic/pituitary radiation dose of 20 Gy to 30 Gy (RR, 1.17; 95% CI, 1.05-1.3; P = .01).
- Specific antidepressant use (paroxetine) (RR, 1.29; 95% CI, 1.08-1.54).
Survivors who adhered to the U.S. Centers for Disease Control and Prevention guidelines for vigorous physical activity (RR, 0.90; 95% CI, 0.82-0.97; P = .01) and who had a medium amount of anxiety (RR, 0.86; 95% CI, 0.75-0.99; P = .04) had a lower risk of obesity.[104] The development of obesity after cranial radiation therapy is multifactorial and includes the following:[93,105,106] - GHD.
- Leptin sensitivity.
- Reduced levels of physical activity and energy expenditure.
Body composition alterations after childhood ALL Moderate-dose cranial radiation therapy (18-24 Gy) among ALL survivors is associated with obesity, particularly in females treated at a young age.[72,91,93,107] Female adult survivors of childhood ALL who were treated with cranial radiation therapy of 24 Gy before age 5 years are four times more likely to be obese than are women who have not been treated for a cancer.[91] In addition, women treated with 18 Gy to 24 Gy cranial radiation therapy before age 10 years have a substantially greater rate of increase in their BMI through their young adult years than do women who were treated for ALL with only chemotherapy or women in the general population.[93] It appears that these women also have a significantly increased visceral adiposity and associated insulin resistance.[108,109] These outcomes are attenuated in males. However, a study of long-term male survivors of ALL (mean age, 29 years) observed significantly higher body adiposity than in age-matched controls, despite normal weight and BMI. Potential indicators of increased adiposity included high leptin and low sex hormone-binding globulin levels. Serum testicular endocrine markers (testosterone, FSH, or inhibin B) did not correlate with body adiposity.[110] ALL therapy regimens are associated with increases in BMI shortly after completion of therapy, and possibly with a higher risk of obesity in the long term.[94,95,96,111,112] Several studies have reported that survivors of childhood ALL treated with chemotherapy alone also exhibit long-term changes in body composition, with relative increases in body fat [109,113,114,115] and visceral adiposity in comparison to lean mass.[108] These changes cannot be detected if BMI alone is used in the assessment of metabolic risk in this population. A cohort study of 365 adult survivors of ALL (149 treated with cranial radiation therapy and 216 treated without cranial radiation therapy) that compared body composition, energy balance, and fitness to age-, sex-, and race-matched peers disclosed that female survivors who were not exposed to cranial irradiation had comparable body composition values to that of peers. However, waist circumference, waist-to-height ratio, and total and percent fat mass were higher among male survivors and cranial radiation-exposed female survivors than among comparison group members. Survivors of both sexes exposed to cranial radiation therapy had higher BMI and percent body fat than did survivors not exposed to cranial radiation therapy. Although survivors who did not receive cranial radiation therapy had energy balance similar to the matched peer group, they had significantly higher measures of impaired fitness (impaired flexibility, peripheral sensorimotor deficits, proximal muscle weakness, and poor exercise tolerance). These results suggest that elimination of cranial radiation from ALL therapy has improved, but not eliminated, adverse body composition outcomes and underscores the importance of attention to interventions to preserve function in this group as they age.[116] In contrast, in a report from the CCSS, adult survivors of childhood ALL treated with chemotherapy alone did not have significantly higher rates of obesity than did sibling controls,[91] nor were there differences in BMI changes between these groups after a subsequent period of follow-up that averaged 7.8 years.[93] Results from the CCSS, however, were based on self-reported height and weight measurements. Likewise, COG investigators also did not observe an increased risk of being overweight and obese based on BMI measurements in 269 patients with standard-risk ALL (age, 3.5 years at diagnosis and 13.3 years at follow-up) compared with peers without cancer. Again, these variable outcomes likely relate to the use of BMI as the metric for abnormal body composition, which does not adequately assess visceral adiposity that can contribute to metabolic risk in this population.[117] Body composition alterations after treatment for CNS tumors Among brain tumor survivors treated with higher doses of cranial radiation therapy, only females treated at a younger age appear to be at increased risk for obesity.[118] Body composition alterations after hematopoietic cell transplantation Survivors of childhood cancer treated with TBI in preparation for an allogeneic HSCT have increased measures of body fatness (percent fat) while often having a normal BMI.[81,85,119] Longitudinal decline in BMI related to substantial decrease in lean mass has been observed among survivors of hematological malignancies treated with allogeneic HSCT. This finding was largely attributable to TBI conditioning and severity of chronic GVHD.[120] Body composition and frailty Young adult childhood cancer survivors have a higher-than-expected prevalence of frailty, a phenotype characterized by low muscle mass, self-reported exhaustion, low energy expenditure, slow walking speed, and weakness. Individuals are termed prefrail if they have two of these five characteristics and frail if they have three or more of these characteristics. The frailty phenotype increases in prevalence with aging, and has been associated with excess risk of mortality and onset of chronic conditions. Ongoing research aims to elucidate the pathophysiology of frailty and develop/test interventions to prevent or reverse this condition.[121] Table 11. Body Composition Late Effectsa| Predisposing Therapy | Potential Late Effects | Health Screening |
|---|
| BMI = body mass index. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Cranial radiation therapy | Overweight/obesity | Height, weight, BMI, blood pressure | | Labs: fasting glucose and lipids | Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for endocrine and metabolic syndrome late effects information, including risk factors, evaluation, and health counseling. References:
-
Brignardello E, Felicetti F, Castiglione A, et al.: Endocrine health conditions in adult survivors of childhood cancer: the need for specialized adult-focused follow-up clinics. Eur J Endocrinol 168 (3): 465-72, 2013.
-
Mostoufi-Moab S, Seidel K, Leisenring WM, et al.: Endocrine Abnormalities in Aging Survivors of Childhood Cancer: A Report From the Childhood Cancer Survivor Study. J Clin Oncol 34 (27): 3240-7, 2016.
-
Clement SC, Schouten-van Meeteren AY, Boot AM, et al.: Prevalence and Risk Factors of Early Endocrine Disorders in Childhood Brain Tumor Survivors: A Nationwide, Multicenter Study. J Clin Oncol 34 (36): 4362-4370, 2016.
-
Constine LS, Woolf PD, Cann D, et al.: Hypothalamic-pituitary dysfunction after radiation for brain tumors. N Engl J Med 328 (2): 87-94, 1993.
-
Chemaitilly W, Li Z, Huang S, et al.: Anterior hypopituitarism in adult survivors of childhood cancers treated with cranial radiotherapy: a report from the St Jude Lifetime Cohort study. J Clin Oncol 33 (5): 492-500, 2015.
-
Gleeson HK, Darzy K, Shalet SM: Late endocrine, metabolic and skeletal sequelae following treatment of childhood cancer. Best Pract Res Clin Endocrinol Metab 16 (2): 335-48, 2002.
-
Bölling T, Geisenheiser A, Pape H, et al.: Hypothyroidism after head-and-neck radiotherapy in children and adolescents: preliminary results of the "Registry for the Evaluation of Side Effects After Radiotherapy in Childhood and Adolescence" (RiSK). Int J Radiat Oncol Biol Phys 81 (5): e787-91, 2011.
-
Sklar C, Whitton J, Mertens A, et al.: Abnormalities of the thyroid in survivors of Hodgkin's disease: data from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 85 (9): 3227-32, 2000.
-
Bhatti P, Veiga LH, Ronckers CM, et al.: Risk of second primary thyroid cancer after radiotherapy for a childhood cancer in a large cohort study: an update from the childhood cancer survivor study. Radiat Res 174 (6): 741-52, 2010.
-
Haddy N, El-Fayech C, Guibout C, et al.: Thyroid adenomas after solid cancer in childhood. Int J Radiat Oncol Biol Phys 84 (2): e209-15, 2012.
-
Ronckers CM, Sigurdson AJ, Stovall M, et al.: Thyroid cancer in childhood cancer survivors: a detailed evaluation of radiation dose response and its modifiers. Radiat Res 166 (4): 618-28, 2006.
-
Sigurdson AJ, Ronckers CM, Mertens AC, et al.: Primary thyroid cancer after a first tumour in childhood (the Childhood Cancer Survivor Study): a nested case-control study. Lancet 365 (9476): 2014-23, 2005 Jun 11-17.
-
van Santen HM, Tytgat GA, van de Wetering MD, et al.: Differentiated thyroid carcinoma after 131I-MIBG treatment for neuroblastoma during childhood: description of the first two cases. Thyroid 22 (6): 643-6, 2012.
-
Veiga LH, Lubin JH, Anderson H, et al.: A pooled analysis of thyroid cancer incidence following radiotherapy for childhood cancer. Radiat Res 178 (4): 365-76, 2012.
-
Kovalchik SA, Ronckers CM, Veiga LH, et al.: Absolute risk prediction of second primary thyroid cancer among 5-year survivors of childhood cancer. J Clin Oncol 31 (1): 119-27, 2013.
-
Vivanco M, Dalle JH, Alberti C, et al.: Malignant and benign thyroid nodules after total body irradiation preceding hematopoietic cell transplantation during childhood. Eur J Endocrinol 167 (2): 225-33, 2012.
-
Li Z, Franklin J, Zelcer S, et al.: Ultrasound surveillance for thyroid malignancies in survivors of childhood cancer following radiotherapy: a single institutional experience. Thyroid 24 (12): 1796-805, 2014.
-
Brignardello E, Felicetti F, Castiglione A, et al.: Ultrasound surveillance for radiation-induced thyroid carcinoma in adult survivors of childhood cancer. Eur J Cancer 55: 74-80, 2016.
-
Metzger ML, Howard SC, Hudson MM, et al.: Natural history of thyroid nodules in survivors of pediatric Hodgkin lymphoma. Pediatr Blood Cancer 46 (3): 314-9, 2006.
-
Francis GL, Waguespack SG, Bauer AJ, et al.: Management Guidelines for Children with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 25 (7): 716-59, 2015.
-
Sanders JE, Hoffmeister PA, Woolfrey AE, et al.: Thyroid function following hematopoietic cell transplantation in children: 30 years' experience. Blood 113 (2): 306-8, 2009.
-
Gurney JG, Kadan-Lottick NS, Packer RJ, et al.: Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors: Childhood Cancer Survivor Study. Cancer 97 (3): 663-73, 2003.
-
Sklar CA: Growth and neuroendocrine dysfunction following therapy for childhood cancer. Pediatr Clin North Am 44 (2): 489-503, 1997.
-
Hudson MM, Ness KK, Gurney JG, et al.: Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309 (22): 2371-81, 2013.
-
Ramelli GP, von der Weid N, Stanga Z, et al.: Suprasellar germinomas in childhood and adolescence: diagnostic pitfalls. J Pediatr Endocrinol Metab 11 (6): 693-7, 1998 Nov-Dec.
-
Vinchon M, Baroncini M, Leblond P, et al.: Morbidity and tumor-related mortality among adult survivors of pediatric brain tumors: a review. Childs Nerv Syst 27 (5): 697-704, 2011.
-
Fahrner B, Prosch H, Minkov M, et al.: Long-term outcome of hypothalamic pituitary tumors in Langerhans cell histiocytosis. Pediatr Blood Cancer 58 (4): 606-10, 2012.
-
Darzy KH, Shalet SM: Hypopituitarism following radiotherapy. Pituitary 12 (1): 40-50, 2009.
-
Mulder RL, Kremer LC, van Santen HM, et al.: Prevalence and risk factors of radiation-induced growth hormone deficiency in childhood cancer survivors: a systematic review. Cancer Treat Rev 35 (7): 616-32, 2009.
-
Merchant TE, Goloubeva O, Pritchard DL, et al.: Radiation dose-volume effects on growth hormone secretion. Int J Radiat Oncol Biol Phys 52 (5): 1264-70, 2002.
-
Merchant TE, Rose SR, Bosley C, et al.: Growth hormone secretion after conformal radiation therapy in pediatric patients with localized brain tumors. J Clin Oncol 29 (36): 4776-80, 2011.
-
Sklar C, Mertens A, Walter A, et al.: Final height after treatment for childhood acute lymphoblastic leukemia: comparison of no cranial irradiation with 1800 and 2400 centigrays of cranial irradiation. J Pediatr 123 (1): 59-64, 1993.
-
Schriock EA, Schell MJ, Carter M, et al.: Abnormal growth patterns and adult short stature in 115 long-term survivors of childhood leukemia. J Clin Oncol 9 (3): 400-5, 1991.
-
Chow EJ, Friedman DL, Yasui Y, et al.: Decreased adult height in survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Pediatr 150 (4): 370-5, 375.e1, 2007.
-
Vandecruys E, Dhooge C, Craen M, et al.: Longitudinal linear growth and final height is impaired in childhood acute lymphoblastic leukemia survivors after treatment without cranial irradiation. J Pediatr 163 (1): 268-73, 2013.
-
Ogilvy-Stuart AL, Clark DJ, Wallace WH, et al.: Endocrine deficit after fractionated total body irradiation. Arch Dis Child 67 (9): 1107-10, 1992.
-
Willi SM, Cooke K, Goldwein J, et al.: Growth in children after bone marrow transplantation for advanced neuroblastoma compared with growth after transplantation for leukemia or aplastic anemia. J Pediatr 120 (5): 726-32, 1992.
-
Wingard JR, Plotnick LP, Freemer CS, et al.: Growth in children after bone marrow transplantation: busulfan plus cyclophosphamide versus cyclophosphamide plus total body irradiation. Blood 79 (4): 1068-73, 1992.
-
Bernard F, Bordigoni P, Simeoni MC, et al.: Height growth during adolescence and final height after haematopoietic SCT for childhood acute leukaemia: the impact of a conditioning regimen with BU or TBI. Bone Marrow Transplant 43 (8): 637-42, 2009.
-
Chemaitilly W, Sklar CA: Endocrine complications of hematopoietic stem cell transplantation. Endocrinol Metab Clin North Am 36 (4): 983-98; ix, 2007.
-
Huma Z, Boulad F, Black P, et al.: Growth in children after bone marrow transplantation for acute leukemia. Blood 86 (2): 819-24, 1995.
-
Socié G, Salooja N, Cohen A, et al.: Nonmalignant late effects after allogeneic stem cell transplantation. Blood 101 (9): 3373-85, 2003.
-
Cohen A, Rovelli A, Bakker B, et al.: Final height of patients who underwent bone marrow transplantation for hematological disorders during childhood: a study by the Working Party for Late Effects-EBMT. Blood 93 (12): 4109-15, 1999.
-
Raman S, Grimberg A, Waguespack SG, et al.: Risk of Neoplasia in Pediatric Patients Receiving Growth Hormone Therapy--A Report From the Pediatric Endocrine Society Drug and Therapeutics Committee. J Clin Endocrinol Metab 100 (6): 2192-203, 2015.
-
Chemaitilly W, Robison LL: Safety of growth hormone treatment in patients previously treated for cancer. Endocrinol Metab Clin North Am 41 (4): 785-92, 2012.
-
Sklar CA, Mertens AC, Mitby P, et al.: Risk of disease recurrence and second neoplasms in survivors of childhood cancer treated with growth hormone: a report from the Childhood Cancer Survivor Study. J Clin Endocrinol Metab 87 (7): 3136-41, 2002.
-
Ergun-Longmire B, Mertens AC, Mitby P, et al.: Growth hormone treatment and risk of second neoplasms in the childhood cancer survivor. J Clin Endocrinol Metab 91 (9): 3494-8, 2006.
-
Bogarin R, Steinbok P: Growth hormone treatment and risk of recurrence or progression of brain tumors in children: a review. Childs Nerv Syst 25 (3): 273-9, 2009.
-
Patterson BC, Chen Y, Sklar CA, et al.: Growth hormone exposure as a risk factor for the development of subsequent neoplasms of the central nervous system: a report from the childhood cancer survivor study. J Clin Endocrinol Metab 99 (6): 2030-7, 2014.
-
Nandagopal R, Laverdière C, Mulrooney D, et al.: Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res 69 (2): 65-74, 2008.
-
Chemaitilly W, Sklar CA: Endocrine complications in long-term survivors of childhood cancers. Endocr Relat Cancer 17 (3): R141-59, 2010.
-
Chemaitilly W, Merchant TE, Li Z, et al.: Central precocious puberty following the diagnosis and treatment of paediatric cancer and central nervous system tumours: presentation and long-term outcomes. Clin Endocrinol (Oxf) 84 (3): 361-71, 2016.
-
Gan HW, Phipps K, Aquilina K, et al.: Neuroendocrine Morbidity After Pediatric Optic Gliomas: A Longitudinal Analysis of 166 Children Over 30 Years. J Clin Endocrinol Metab 100 (10): 3787-99, 2015.
-
Didcock E, Davies HA, Didi M, et al.: Pubertal growth in young adult survivors of childhood leukemia. J Clin Oncol 13 (10): 2503-7, 1995.
-
Shalet SM, Crowne EC, Didi MA, et al.: Irradiation-induced growth failure. Baillieres Clin Endocrinol Metab 6 (3): 513-26, 1992.
-
Greulich WW, Pyle SI: Radiographic Atlas of Skeletal Development of Hand and Wrist. 2nd ed. Stanford, Ca: Stanford University Press, 1959.
-
Gleeson HK, Stoeter R, Ogilvy-Stuart AL, et al.: Improvements in final height over 25 years in growth hormone (GH)-deficient childhood survivors of brain tumors receiving GH replacement. J Clin Endocrinol Metab 88 (8): 3682-9, 2003.
-
Chow EJ, Friedman DL, Yasui Y, et al.: Timing of menarche among survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer 50 (4): 854-8, 2008.
-
Armstrong GT, Whitton JA, Gajjar A, et al.: Abnormal timing of menarche in survivors of central nervous system tumors: A report from the Childhood Cancer Survivor Study. Cancer 115 (11): 2562-70, 2009.
-
Laughton SJ, Merchant TE, Sklar CA, et al.: Endocrine outcomes for children with embryonal brain tumors after risk-adapted craniospinal and conformal primary-site irradiation and high-dose chemotherapy with stem-cell rescue on the SJMB-96 trial. J Clin Oncol 26 (7): 1112-8, 2008.
-
Rose SR: Cranial irradiation and central hypothyroidism. Trends Endocrinol Metab 12 (3): 97-104, 2001.
-
Cheuk DK, Billups CA, Martin MG, et al.: Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117 (1): 197-206, 2011.
-
Rose SR, Lustig RH, Pitukcheewanont P, et al.: Diagnosis of hidden central hypothyroidism in survivors of childhood cancer. J Clin Endocrinol Metab 84 (12): 4472-9, 1999.
-
Paulino AC: Hypothyroidism in children with medulloblastoma: a comparison of 3600 and 2340 cGy craniospinal radiotherapy. Int J Radiat Oncol Biol Phys 53 (3): 543-7, 2002.
-
Patterson BC, Truxillo L, Wasilewski-Masker K, et al.: Adrenal function testing in pediatric cancer survivors. Pediatr Blood Cancer 53 (7): 1302-7, 2009.
-
Kazlauskaite R, Evans AT, Villabona CV, et al.: Corticotropin tests for hypothalamic-pituitary- adrenal insufficiency: a metaanalysis. J Clin Endocrinol Metab 93 (11): 4245-53, 2008.
-
Rose SR, Danish RK, Kearney NS, et al.: ACTH deficiency in childhood cancer survivors. Pediatr Blood Cancer 45 (6): 808-13, 2005.
-
Constine LS, Rubin P, Woolf PD, et al.: Hyperprolactinemia and hypothyroidism following cytotoxic therapy for central nervous system malignancies. J Clin Oncol 5 (11): 1841-51, 1987.
-
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106 (25): 3143-421, 2002.
-
Chow EJ, Simmons JH, Roth CL, et al.: Increased cardiometabolic traits in pediatric survivors of acute lymphoblastic leukemia treated with total body irradiation. Biol Blood Marrow Transplant 16 (12): 1674-81, 2010.
-
Surapolchai P, Hongeng S, Mahachoklertwattana P, et al.: Impaired glucose tolerance and insulin resistance in survivors of childhood acute lymphoblastic leukemia: prevalence and risk factors. J Pediatr Hematol Oncol 32 (5): 383-9, 2010.
-
Veringa SJ, van Dulmen-den Broeder E, Kaspers GJ, et al.: Blood pressure and body composition in long-term survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 58 (2): 278-82, 2012.
-
Steinberger J, Sinaiko AR, Kelly AS, et al.: Cardiovascular risk and insulin resistance in childhood cancer survivors. J Pediatr 160 (3): 494-9, 2012.
-
Gurney JG, Ness KK, Sibley SD, et al.: Metabolic syndrome and growth hormone deficiency in adult survivors of childhood acute lymphoblastic leukemia. Cancer 107 (6): 1303-12, 2006.
-
Nottage KA, Ness KK, Li C, et al.: Metabolic syndrome and cardiovascular risk among long-term survivors of acute lymphoblastic leukaemia - From the St. Jude Lifetime Cohort. Br J Haematol 165 (3): 364-74, 2014.
-
Oudin C, Simeoni MC, Sirvent N, et al.: Prevalence and risk factors of the metabolic syndrome in adult survivors of childhood leukemia. Blood 117 (17): 4442-8, 2011.
-
Armstrong GT, Oeffinger KC, Chen Y, et al.: Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol 31 (29): 3673-80, 2013.
-
Smith WA, Li C, Nottage KA, et al.: Lifestyle and metabolic syndrome in adult survivors of childhood cancer: a report from the St. Jude Lifetime Cohort Study. Cancer 120 (17): 2742-50, 2014.
-
Jones LW, Liu Q, Armstrong GT, et al.: Exercise and risk of major cardiovascular events in adult survivors of childhood hodgkin lymphoma: a report from the childhood cancer survivor study. J Clin Oncol 32 (32): 3643-50, 2014.
-
van Waas M, Neggers SJ, Raat H, et al.: Abdominal radiotherapy: a major determinant of metabolic syndrome in nephroblastoma and neuroblastoma survivors. PLoS One 7 (12): e52237, 2012.
-
Neville KA, Cohn RJ, Steinbeck KS, et al.: Hyperinsulinemia, impaired glucose tolerance, and diabetes mellitus in survivors of childhood cancer: prevalence and risk factors. J Clin Endocrinol Metab 91 (11): 4401-7, 2006.
-
Baker KS, Ness KK, Steinberger J, et al.: Diabetes, hypertension, and cardiovascular events in survivors of hematopoietic cell transplantation: a report from the bone marrow transplantation survivor study. Blood 109 (4): 1765-72, 2007.
-
van Waas M, Neggers SJ, Uitterlinden AG, et al.: Treatment factors rather than genetic variation determine metabolic syndrome in childhood cancer survivors. Eur J Cancer 49 (3): 668-75, 2013.
-
de Vathaire F, El-Fayech C, Ben Ayed FF, et al.: Radiation dose to the pancreas and risk of diabetes mellitus in childhood cancer survivors: a retrospective cohort study. Lancet Oncol 13 (10): 1002-10, 2012.
-
Armenian SH, Chemaitilly W, Chen M, et al.: National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Cardiovascular Disease and Associated Risk Factors Working Group Report. Biol Blood Marrow Transplant 23 (2): 201-210, 2017.
-
Baker KS, Chow EJ, Goodman PJ, et al.: Impact of treatment exposures on cardiovascular risk and insulin resistance in childhood cancer survivors. Cancer Epidemiol Biomarkers Prev 22 (11): 1954-63, 2013.
-
Meacham LR, Chow EJ, Ness KK, et al.: Cardiovascular risk factors in adult survivors of pediatric cancer--a report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev 19 (1): 170-81, 2010.
-
van Santen HM, Geskus RB, Raemaekers S, et al.: Changes in body mass index in long-term childhood cancer survivors. Cancer 121 (23): 4197-204, 2015.
-
Meacham LR, Gurney JG, Mertens AC, et al.: Body mass index in long-term adult survivors of childhood cancer: a report of the Childhood Cancer Survivor Study. Cancer 103 (8): 1730-9, 2005.
-
Mayer EI, Reuter M, Dopfer RE, et al.: Energy expenditure, energy intake and prevalence of obesity after therapy for acute lymphoblastic leukemia during childhood. Horm Res 53 (4): 193-9, 2000.
-
Oeffinger KC, Mertens AC, Sklar CA, et al.: Obesity in adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol 21 (7): 1359-65, 2003.
-
Sklar CA, Mertens AC, Walter A, et al.: Changes in body mass index and prevalence of overweight in survivors of childhood acute lymphoblastic leukemia: role of cranial irradiation. Med Pediatr Oncol 35 (2): 91-5, 2000.
-
Garmey EG, Liu Q, Sklar CA, et al.: Longitudinal changes in obesity and body mass index among adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Clin Oncol 26 (28): 4639-45, 2008.
-
Chow EJ, Pihoker C, Hunt K, et al.: Obesity and hypertension among children after treatment for acute lymphoblastic leukemia. Cancer 110 (10): 2313-20, 2007.
-
Withycombe JS, Post-White JE, Meza JL, et al.: Weight patterns in children with higher risk ALL: A report from the Children's Oncology Group (COG) for CCG 1961. Pediatr Blood Cancer 53 (7): 1249-54, 2009.
-
Dalton VK, Rue M, Silverman LB, et al.: Height and weight in children treated for acute lymphoblastic leukemia: relationship to CNS treatment. J Clin Oncol 21 (15): 2953-60, 2003.
-
Nathan PC, Jovcevska V, Ness KK, et al.: The prevalence of overweight and obesity in pediatric survivors of cancer. J Pediatr 149 (4): 518-25, 2006.
-
Sahakitrungruang T, Klomchan T, Supornsilchai V, et al.: Obesity, metabolic syndrome, and insulin dynamics in children after craniopharyngioma surgery. Eur J Pediatr 170 (6): 763-9, 2011.
-
Müller HL: Childhood craniopharyngioma--current concepts in diagnosis, therapy and follow-up. Nat Rev Endocrinol 6 (11): 609-18, 2010.
-
Müller HL: Childhood craniopharyngioma: current controversies on management in diagnostics, treatment and follow-up. Expert Rev Neurother 10 (4): 515-24, 2010.
-
Simoneau-Roy J, O'Gorman C, Pencharz P, et al.: Insulin sensitivity and secretion in children and adolescents with hypothalamic obesity following treatment for craniopharyngioma. Clin Endocrinol (Oxf) 72 (3): 364-70, 2010.
-
May JA, Krieger MD, Bowen I, et al.: Craniopharyngioma in childhood. Adv Pediatr 53: 183-209, 2006.
-
Müller HL, Gebhardt U, Teske C, et al.: Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after 3-year follow-up. Eur J Endocrinol 165 (1): 17-24, 2011.
-
Green DM, Cox CL, Zhu L, et al.: Risk factors for obesity in adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 30 (3): 246-55, 2012.
-
Oeffinger KC: Are survivors of acute lymphoblastic leukemia (ALL) at increased risk of cardiovascular disease? Pediatr Blood Cancer 50 (2 Suppl): 462-7; discussion 468, 2008.
-
Brennan BM, Rahim A, Blum WF, et al.: Hyperleptinaemia in young adults following cranial irradiation in childhood: growth hormone deficiency or leptin insensitivity? Clin Endocrinol (Oxf) 50 (2): 163-9, 1999.
-
Didi M, Didcock E, Davies HA, et al.: High incidence of obesity in young adults after treatment of acute lymphoblastic leukemia in childhood. J Pediatr 127 (1): 63-7, 1995.
-
Janiszewski PM, Oeffinger KC, Church TS, et al.: Abdominal obesity, liver fat, and muscle composition in survivors of childhood acute lymphoblastic leukemia. J Clin Endocrinol Metab 92 (10): 3816-21, 2007.
-
Oeffinger KC, Adams-Huet B, Victor RG, et al.: Insulin resistance and risk factors for cardiovascular disease in young adult survivors of childhood acute lymphoblastic leukemia. J Clin Oncol 27 (22): 3698-704, 2009.
-
Jahnukainen K, Heikkinen R, Henriksson M, et al.: Increased Body Adiposity and Serum Leptin Concentrations in Very Long-Term Adult Male Survivors of Childhood Acute Lymphoblastic Leukemia. Horm Res Paediatr 84 (2): 108-15, 2015.
-
Kohler JA, Moon RJ, Wright S, et al.: Increased adiposity and altered adipocyte function in female survivors of childhood acute lymphoblastic leukaemia treated without cranial radiation. Horm Res Paediatr 75 (6): 433-40, 2011.
-
Zhang FF, Rodday AM, Kelly MJ, et al.: Predictors of being overweight or obese in survivors of pediatric acute lymphoblastic leukemia (ALL). Pediatr Blood Cancer 61 (7): 1263-9, 2014.
-
Warner JT, Evans WD, Webb DK, et al.: Body composition of long-term survivors of acute lymphoblastic leukaemia. Med Pediatr Oncol 38 (3): 165-72, 2002.
-
Miller TL, Lipsitz SR, Lopez-Mitnik G, et al.: Characteristics and determinants of adiposity in pediatric cancer survivors. Cancer Epidemiol Biomarkers Prev 19 (8): 2013-22, 2010.
-
Jarfelt M, Lannering B, Bosaeus I, et al.: Body composition in young adult survivors of childhood acute lymphoblastic leukaemia. Eur J Endocrinol 153 (1): 81-9, 2005.
-
Ness KK, DeLany JP, Kaste SC, et al.: Energy balance and fitness in adult survivors of childhood acute lymphoblastic leukemia. Blood 125 (22): 3411-9, 2015.
-
Lindemulder SJ, Stork LC, Bostrom B, et al.: Survivors of standard risk acute lymphoblastic leukemia do not have increased risk for overweight and obesity compared to non-cancer peers: a report from the Children's Oncology Group. Pediatr Blood Cancer 62 (6): 1035-41, 2015.
-
Gurney JG, Ness KK, Stovall M, et al.: Final height and body mass index among adult survivors of childhood brain cancer: childhood cancer survivor study. J Clin Endocrinol Metab 88 (10): 4731-9, 2003.
-
Nysom K, Holm K, Michaelsen KF, et al.: Degree of fatness after allogeneic BMT for childhood leukaemia or lymphoma. Bone Marrow Transplant 27 (8): 817-20, 2001.
-
Inaba H, Yang J, Kaste SC, et al.: Longitudinal changes in body mass and composition in survivors of childhood hematologic malignancies after allogeneic hematopoietic stem-cell transplantation. J Clin Oncol 30 (32): 3991-7, 2012.
-
Ness KK, Krull KR, Jones KE, et al.: Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer: a report from the St Jude Lifetime cohort study. J Clin Oncol 31 (36): 4496-503, 2013.
Late Effects of the Immune SystemLate effects of the immune system have not been well studied, especially in survivors treated with contemporary therapies. Reports published about long-term immune system outcomes are limited by retrospective data collection, small sample size, cohort selection and participation bias, heterogeneity in treatment approach, time since treatment, and method of ascertainment. Asplenia Surgical or functional splenectomy increases the risk of life-threatening invasive bacterial infection:[1] - Although staging laparotomy is no longer standard practice for pediatric Hodgkin lymphoma, patients from earlier time periods have ongoing risks.[2,3]
- Children may be rendered asplenic by radiation therapy to the spleen in doses greater than 30 Gy.[4,5] Low-dose involved-field radiation therapy (21 Gy) combined with multiagent chemotherapy did not appear to adversely affect splenic function, as measured by pitted red blood cell assays.[5] No other studies of immune status after radiation therapy are available.
- Functional asplenia (with Howell-Jolly bodies, reduced splenic size and blood flow) after hematopoietic stem cell transplantation (HSCT) has been attributed to graft-versus-host disease (GVHD).
Individuals with asplenia, regardless of the reason for the asplenic state, have an increased risk of fulminant bacteremia, especially associated with encapsulated bacteria, which is associated with a high mortality rate. The risk of bacteremia is higher in younger children than in older children, and this risk may be greater during the years immediately after splenectomy. Fulminant septicemia, however, has been reported in adults up to 25 years after splenectomy. Bacteremia may be caused by the following organisms: - Streptococcus pneumoniae. The most common pathogen that causes bacteremia in children with asplenia.
- Other streptococci.
- Haemophilus influenzae type b (Hib).
- Neisseria meningitidis.
- Escherichia coli; Staphylococcus aureus.
- Gram-negative bacilli, such as the Salmonella species, the Klebsiella species, and Pseudomonas aeruginosa.
Individuals with functional or surgical asplenia are also at increased risk of fatal malaria and severe babesiosis. Posttherapy management Clinicians should consider and encourage the administration of inactivated vaccines (e.g., influenza) and vaccines made of purified antigens (e.g., pneumococcus), bacterial components (e.g., diphtheria-tetanus-pertussis), or genetically engineered recombinant antigens (e.g., hepatitis B) in all cancer and transplant survivors according to recommended doses and schedules.[6,7,8] Two primary doses of quadrivalent meningococcal conjugate vaccine should be administered 2 months apart to children with asplenia, from age 2 years through adolescence, and a booster dose should be administered every 5 years.[9] (Refer to the Scheduling Immunizations section of the Red Book for more information.) However, the efficacy of meningococcal vaccines in children with asplenia has not been established. (Refer to the Meningococcal Infections section of the Red Book for more information.) No known contraindication exists to giving these vaccines at the same time as other required vaccines, in separate syringes, at different sites. Pneumococcal conjugate vaccine (PCV) and pneumococcal polysaccharide vaccine (PPSV) are indicated at the recommended age for all children with asplenia. Following the administration of the appropriate number of doses of PCV13, PPSV23 should be administered starting at age 24 months. A second dose should be administered 5 years later. For children aged 2 to 5 years with a complete PCV7 series who have not received PCV13, a supplemental dose of PCV13 should be administered. For asplenic individuals aged 6 to 18 years who have not received a dose of PCV13, a supplemental dose of PCV13 should be considered.[10] (Refer to the Pneumococcal Infections section of the Red Book for more information.) Hib immunization should be initiated at age 2 months, which is recommended for otherwise healthy young children and for all previously unimmunized children with asplenia.[10] (Refer to the Scheduling Immunizations section of the Red Book for more information.) Daily antimicrobial prophylaxis against pneumococcal infections is recommended for many children with asplenia, regardless of their immunization status. Although the efficacy of antimicrobial prophylaxis has been proven only in patients with sickle cell anemia, other children with asplenia at particularly high risk, such as children with malignant neoplasms or thalassemia, should also receive daily chemoprophylaxis. In general, antimicrobial prophylaxis (in addition to immunization) should be considered for all children with asplenia younger than 5 years and for at least 1 year after splenectomy. The age at which chemoprophylaxis is discontinued is often an empiric decision. On the basis of a multicenter study, prophylactic penicillin can be discontinued at age 5 years in children with sickle cell disease who are receiving regular medical attention and who have not had a severe pneumococcal infection or surgical splenectomy. The appropriate duration of prophylaxis is unknown for children with asplenia attributable to other causes. Some experts continue prophylaxis throughout childhood and into adulthood for particularly high-risk patients with asplenia. Table 12. Spleen Late Effectsa| Predisposing Therapy | Immunologic Effects | Health Screening/Interventions |
|---|
| GVHD = graft-versus-host disease; HSCT = hematopoietic stem cell transplantation; IgA = immunoglobulin A; T = temperature. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Radiation impacting spleen; splenectomy; HSCT with currently active GVHD | Asplenia/hyposplenia; overwhelming post-splenectomy sepsis | Blood cultures during febrile episodes (T >38.5°C); empiric antibiotics | | HSCT with any history of chronic GVHD | Immunologic complications (secretory IgA deficiency, hypogammaglobulinemia, decreased B cells, T cell dysfunction, chronic infections [e.g., conjunctivitis, sinusitis, and bronchitis associated with chronic GVHD]) | History: chronic conjunctivitis, chronic sinusitis, chronic bronchitis, recurrent or unusual infections, sepsis | | Exam: attention to eyes, nose/sinuses, and lungs | Refer to the Centers for Disease Control and Prevention (CDC) Guidelines for Preventing Opportunistic Infections Among Hematopoietic Stem Cell Transplant Recipients for more information on posttransplant immunization. Humoral Immunity Although the immune system appears to recover from the effects of active chemotherapy and radiation therapy, there is some evidence that lymphoid subsets may not always normalize. Innate immunity, thymopoiesis, and DNA damage responses to radiation were shown to be abnormal in survivors of childhood leukemia.[11] Defects in immune recovery characterized by B-cell depletion have been observed in 2-year survivors of standard-risk and intermediate-risk acute lymphoblastic leukemia (ALL).[12] Antibody levels to previous vaccinations are also reduced in patients off therapy for ALL for at least 1 year,[13,14] suggesting persistence of abnormal humoral immunity [15] and a need for revaccination in such children. Many survivors of childhood cancer will remain susceptible to vaccine-preventable infections. While there is a paucity of data regarding the benefits of administering active immunizations in this population, reimmunization is necessary to provide protective antibodies. The recommended reimmunization schedule will depend on previously received vaccinations and on the intensity of therapy.[16,17] In some children who received intensive treatment, consideration may be given to evaluating the antibodies against common vaccination antigens to determine the need for revaccination. (Refer to the Scheduling Immunizations section of the Red Book for more information.) Immune status is also compromised after HSCT, particularly in association with GVHD.[18] In a prospective, longitudinal study of 210 survivors treated with allogeneic HSCT, antibody responses lasting for more than 5 years after immunization were observed in most patients for tetanus (95.7%), rubella (92.3%), poliovirus (97.9%), and, in diphtheria-tetanus-acellular pertussis (DTaP) recipients, diphtheria (100%). However, responses to pertussis (25.0%), measles (66.7%), mumps (61.5%), hepatitis B (72.9%), and diphtheria in tetanus-diphtheria (Td) recipients (48.6%) were less favorable. Factors associated with vaccine failure include older age at immunization; lower CD3, CD4, or CD19 count; higher immunoglobulin M concentration; positive recipient cytomegalovirus serology; negative titer before immunization; history of acute or chronic GVHD; and radiation conditioning.[19] Follow-up recommendations for transplant recipients have been published by the major North American and European transplant groups, the CDC, and the Infectious Diseases Society of America.[20,21] Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for immune system late effects information including risk factors, evaluation, and health counseling. References:
-
Immunization in special circumstances. In: Kimberlin DW, Brady MT, Jackson MA, et al., eds.: Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, Ill: American Academy of Pediatrics, 2015, pp 68-107.
-
Kaiser CW: Complications from staging laparotomy for Hodgkin disease. J Surg Oncol 16 (4): 319-25, 1981.
-
Jockovich M, Mendenhall NP, Sombeck MD, et al.: Long-term complications of laparotomy in Hodgkin's disease. Ann Surg 219 (6): 615-21; discussion 621-4, 1994.
-
Coleman CN, McDougall IR, Dailey MO, et al.: Functional hyposplenia after splenic irradiation for Hodgkin's disease. Ann Intern Med 96 (1): 44-7, 1982.
-
Weiner MA, Landmann RG, DeParedes L, et al.: Vesiculated erythrocytes as a determination of splenic reticuloendothelial function in pediatric patients with Hodgkin's disease. J Pediatr Hematol Oncol 17 (4): 338-41, 1995.
-
National Center for Immunization and Respiratory Diseases: General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 60 (RR02): 1-60, 2011. Available online Last accessed April 14, 2017.
-
Bridges CB, Coyne-Beasley T; Advisory Committee on Immunization Practices: Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older: United States, 2014. Ann Intern Med 160 (3): 190, 2014.
-
Rubin LG, Levin MJ, Ljungman P, et al.: 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis 58 (3): 309-18, 2014.
-
Centers for Disease Control and Prevention (CDC): Recommendation of the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MenACWY-D) among children aged 9 through 23 months at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep 60 (40): 1391-2, 2011.
-
Kimberlin DW, Brady MT, Jackson MA, et al., eds.: Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, Ill: American Academy of Pediatrics, 2015. Also available online. Last accessed April 14, 2017.
-
Schwartz C L, Hobbie WL, Constine LS, et al., eds.: Survivors of Childhood Cancer: Assessment and Management. St. Louis, Mo: Mosby, 1994.
-
Koskenvuo M, Ekman I, Saha E, et al.: Immunological Reconstitution in Children After Completing Conventional Chemotherapy of Acute Lymphoblastic Leukemia is Marked by Impaired B-cell Compartment. Pediatr Blood Cancer 63 (9): 1653-6, 2016.
-
Leung W, Neale G, Behm F, et al.: Deficient innate immunity, thymopoiesis, and gene expression response to radiation in survivors of childhood acute lymphoblastic leukemia. Cancer Epidemiol 34 (3): 303-8, 2010.
-
Aytac S, Yalcin SS, Cetin M, et al.: Measles, mumps, and rubella antibody status and response to immunization in children after therapy for acute lymphoblastic leukemia. Pediatr Hematol Oncol 27 (5): 333-43, 2010.
-
Brodtman DH, Rosenthal DW, Redner A, et al.: Immunodeficiency in children with acute lymphoblastic leukemia after completion of modern aggressive chemotherapeutic regimens. J Pediatr 146 (5): 654-61, 2005.
-
Ruggiero A, Battista A, Coccia P, et al.: How to manage vaccinations in children with cancer. Pediatr Blood Cancer 57 (7): 1104-8, 2011.
-
Patel SR, Chisholm JC, Heath PT: Vaccinations in children treated with standard-dose cancer therapy or hematopoietic stem cell transplantation. Pediatr Clin North Am 55 (1): 169-86, xi, 2008.
-
Olkinuora HA, Taskinen MH, Saarinen-Pihkala UM, et al.: Multiple viral infections post-hematopoietic stem cell transplantation are linked to the appearance of chronic GVHD among pediatric recipients of allogeneic grafts. Pediatr Transplant 14 (2): 242-8, 2010.
-
Inaba H, Hartford CM, Pei D, et al.: Longitudinal analysis of antibody response to immunization in paediatric survivors after allogeneic haematopoietic stem cell transplantation. Br J Haematol 156 (1): 109-17, 2012.
-
Rizzo JD, Wingard JR, Tichelli A, et al.: Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, Center for International Blood and Marrow Transplant Research, and the American Society for Blood and Marrow Transplantation (EBMT/CIBMTR/ASBMT). Bone Marrow Transplant 37 (3): 249-61, 2006.
-
Tomblyn M, Chiller T, Einsele H, et al.: Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant 15 (10): 1143-238, 2009.
Late Effects of the Musculoskeletal SystemThe musculoskeletal system of growing children and adolescents is vulnerable to the cytotoxic effects of cancer therapies, including surgery, chemotherapy, and radiation therapy. Documented late effects include the following: - Bone and joint (abnormal bone and/or muscle growth) problems.
- Deformity and functional loss associated with amputation/limb-sparing surgery, joint contracture, osteoporosis/fractures, and osteonecrosis.
- Changes in body composition (obesity and loss of lean muscle mass).
While these late effects are discussed individually, it is important to remember that the components of the musculoskeletal system are interrelated. For example, hypoplasia to a muscle group can negatively affect the function of the long bones and the resultant dysfunction can subsequently lead to disuse and osteoporosis. The major strength of the published literature documenting musculoskeletal late effects among children and adolescents treated for cancer is that most studies have clearly defined outcomes and exposures. However, many studies are observational and cross-sectional or retrospective in design. Single-institution studies are common, and for some outcomes, only small convenience cohorts have been described. Thus, it is possible that studies either excluded patients with the most severe musculoskeletal effects because of death or inability to participate in follow-up testing, or oversampled those with the most severe musculoskeletal late effects because these patients were accessible because they returned for complication-related follow-up. Additionally, some of the results reported in adult survivors of childhood cancer may not be relevant to patients currently being treated because the delivery of anticancer modalities, particularly radiation therapy, has changed over the years in response to documented toxicities.[1,2] Bone and Joint Abnormal bone growth Radiation to the head and brain In an age- and dose-dependent fashion, radiation can inhibit normal bone and muscle maturation and development. Radiation to the head (e.g., cranial, orbital, infratemporal, or nasopharyngeal radiation therapy) can cause craniofacial abnormalities, particularly in children treated before age 5 years or with radiation doses of 20 Gy or more.[3,4,5,6,7] Soft tissue sarcomas such as orbital rhabdomyosarcoma and retinoblastoma are two of the more common cancer groups treated with these radiation fields. Often, in addition to the cosmetic impact of the craniofacial abnormalities, there can be related dental and sinus problems. Cranial radiation therapy damages the hypothalamic-pituitary axis in an age- and dose-response fashion, and can result in growth hormone deficiency (GHD).[8,9] If untreated during the growing years, and sometimes, even with appropriate treatment, it leads to a substantially lower final height. Patients with a central nervous system tumor [8,10] or acute lymphoblastic leukemia (ALL) [11,12,13] treated with 18 Gy or more of cranial radiation therapy are at highest risk. Also, patients treated with total-body irradiation (TBI), particularly single-fraction TBI, are at risk of GHD.[14,15,16,17] In addition, if the spine is also irradiated (e.g., craniospinal radiation therapy for medulloblastoma or early ALL therapies in the 1960s), growth can be affected by two separate mechanisms-GHD and direct damage to the spine. Radiation to the spine and long bones Radiation therapy can also directly affect the growth of the spine and long bones (and associated muscle groups) and can cause premature closure of the epiphyses, leading to the following:[18,19,20,21,22,23,24] - Short stature.
- Asymmetric growth (scoliosis/kyphosis).
- Limb-length discrepancy.
Orthovoltage radiation therapy, commonly used before 1970, delivered high doses of radiation to bone and was commonly associated with subsequent abnormalities in bone growth. However, even with contemporary radiation therapy, if a solid tumor is located near an epiphysis or the spine, alterations in normal bone development can be difficult to avoid. The effects of radiation therapy administered to the spine on stature in survivors of Wilms tumor have been assessed. - In the National Wilms Tumor Study (NWTS), studies 1 through 4, stature loss in 2,778 children was evaluated.[19] Repeated height measurements were collected during long-term follow-up. The effects of radiation dosage, age at treatment, and chemotherapy on stature were analyzed using statistical models that accounted for the normal variation in height with gender and advancing age. Predictions from the model were validated by descriptive analysis of heights measured at ages 17 to 18 years for 205 patients. For those younger than 12 months at diagnosis who received more than 10 Gy, the estimated adult-height deficit was 7.7 cm when contrasted with the nonradiation therapy group. For those who received 10 Gy, the estimated trunk shortening was 2.8 cm or less. Among those whose height measurements in the teenage years were available, patients who received more than 15 Gy of radiation therapy were 4 to 7 cm shorter on average than their nonirradiated counterparts, with a dose-response relationship evident. Chemotherapy did not confer additional risk.
- The effect of radiation therapy on the development of scoliosis has also been re-evaluated. In a group of 42 children treated for Wilms tumor from 1968 to 1994, scoliosis was seen in 18 patients, with only one patient needing orthopedic intervention.[25] Median time to development of scoliosis was 102 months (range, 16-146 months). A clear dose-response relationship was seen; children treated with lower dosages (<24 Gy) of radiation had a significantly lower incidence of scoliosis than those who received more than 24 Gy of radiation. There was also a suggestion that the incidence was lower in patients who received 10 to 12 Gy, the dosages currently used for Wilms tumor, although the sample size was small.
Osteoporosis/fractures Maximal peak bone mass is an important factor influencing the risk of osteoporosis and fracture associated with aging. Treatment-related factors that affect bone mineral loss include the following: - Chemotherapy. Methotrexate has a cytotoxic effect on osteoblasts, resulting in a reduction of bone volume and formation of new bone.[26,27] This effect may be exacerbated by the chronic use of corticosteroids, another class of agents routinely used in the treatment of hematological malignancies and in supportive care for a variety of pediatric cancers.
- Radiation therapy. Radiation-related endocrinopathies, such as GHD or hypogonadism, may contribute to ongoing bone mineral loss.[28,29]
- Suboptimal nutrition and physical inactivity may further predispose to deficits in bone mineral accretion.
Most of our knowledge about cancer and treatment effects on bone mineralization has been derived from studies of children with ALL.[26,30] In this group, the leukemic process, and possibly vitamin D deficiency, may play a role in the alterations in bone metabolism and bone mass observed at diagnosis.[31] Antileukemic therapy causes further bone mineral density loss,[32] which has been reported to normalize over time [33,34] or to persist for many years after completion of therapy.[35,36] Clinical factors predicting higher risk of low bone mineral density include treatment with high cumulative doses of methotrexate (>40 g/m2), high cumulative doses of corticosteroids (>9 g/m2), cranial radiation therapy, or craniospinal radiation therapy, and use of more potent glucocorticoids like dexamethasone.[35,37,38,39,40] Clinical assessment of bone mineral density in adults treated for childhood ALL indicates that most bone mineral deficits normalize over time after discontinuing osteotoxic therapy. Very low bone mineral density was relatively uncommon in a cohort of 845 adult survivors of childhood ALL evaluated at a median age of 31 years, with only 5.7% and 23.8% demonstrating bone mineral density z-scores consistent with osteoporosis and osteopenia, respectively. Cranial radiation dose of 24 Gy or greater, but not cumulative methotrexate or prednisone equivalent doses, was associated with a twofold elevated risk of bone mineral density z-scores of -1 or lower. In a subset of 400 survivors with longitudinal bone mineral density evaluations, bone mineral density z-scores tended to improve from adolescence to young adulthood.[39] Among 862 ALL survivors (median age, 31.3 years) evaluated by quantitative computed tomography of L1 through L2 vertebrae, 30% had low bone mineral density (z score below -1) and 18.6% met criteria for frailty or prefrailty.[41] Modifiable factors such as GHD, smoking, and alcohol consumption were significant predictors for these outcomes, with varying impact on the basis of gender. These data underscore the importance of lifestyle counseling and screening for hormonal deficits during long-term survivors' follow-up evaluations. Bone mineral density deficits that are likely multifactorial in etiology have been reported in allogeneic hematopoietic cell transplant recipients conditioned with TBI.[42,43] French investigators observed a significant risk for lower femoral bone mineral density among adult survivors of childhood leukemia treated with hematopoietic stem cell transplantation (HSCT) who had gonadal deficiency.[44] Hormonal therapy has been shown to enhance bone mineral density of adolescent girls diagnosed with hypogonadism after HSCT.[45][Level of evidence: 3iiiC] Despite disease- and treatment-related risks of bone mineral density deficits, the prevalence of self-reported fractures among Childhood Cancer Survivor Study (CCSS) participants was lower than that reported by sibling controls. Predictors of increased prevalence of fracture by multivariable analyses included the following:[46] - Among female survivors, increasing age at follow-up, white race, methotrexate treatment, and balance difficulties.
- Among male survivors, smoking history and white race.
Radiation-induced fractures can occur with doses of radiation of 50 Gy or greater, as is often used in the treatment of Ewing sarcoma of the extremity.[47,48] Osteonecrosis Osteonecrosis (also known as aseptic or avascular necrosis) is a rare, but well-recognized skeletal complication observed predominantly in survivors of pediatric hematological malignancies treated with corticosteroids.[49,50,51] The prevalence of osteonecrosis has varied from 1% to 22% based on the study population, treatment protocol, method of evaluation, and time from treatment.[51,52,53,54,55,56,57] The condition is characterized by death of one or more segments of bone that most often affects weight-bearing joints, especially the hips and knees. Longitudinal cohort studies have identified a spectrum of clinical manifestations of osteonecrosis, ranging from asymptomatic, spontaneously-resolving imaging changes to painful progressive articular collapse requiring joint replacement.[58,59] Symptomatic osteonecrosis characterized by pain, joint swelling, and reduced mobility typically presents during the first 2 years of therapy, particularly in patients with ALL. These symptoms may improve over time, persist, or progress in the years after completion of therapy. In one series, 60% of patients continued to have symptoms at a median follow-up of 4.9 years after diagnosis of osteonecrosis.[60] Surgical procedures, including core decompression, osteotomy and joint replacements, are sometimes performed in those with persistently severe symptoms.[60] Factors that increase the risk of osteonecrosis include the following: - Exposure to corticosteroids, and possibly methotrexate and concurrent asparaginase. The most important treatment factor associated with the development of osteonecrosis is prolonged exposure to corticosteroids, which is typical in regimens used for ALL, non-Hodgkin lymphoma, and HSCT.[54,57,61,62] Osteonecrosis risk may be related to type of corticosteroid, with some studies in patients with ALL indicating increased risk with the use of dexamethasone compared with prednisone.[63] Corticosteroid dosing schedule also appears to impact the risk of developing osteonecrosis. In the Children's Oncology Group (COG) 1961 trial for newly diagnosed high-risk ALL, patients were randomly assigned to receive either continuous (daily) dexamethasone or an alternate-week schedule of dexamethasone during the delayed intensification phase; the alternate-week schedule was associated with a lower incidence of osteonecrosis.[51] In addition to corticosteroids, exposure to methotrexate and concurrent asparaginase may contribute to the development of osteonecrosis.[64]
- Hematopoietic cell transplantation (HCT) conditioning and course. In a large case-control study that evaluated risk factors for osteonecrosis using data from the Center for International Blood and Marrow Transplant Research, lower risks of osteonecrosis were seen in patients with nonmalignant diseases and in those who had received reduced-intensity conditioning regimens for malignant diseases compared with patients receiving myeloablative regimens for malignant diseases.[65] Several studies have reported an increased risk of osteonecrosis in association with chronic graft-versus-host disease (GVHD).[55,61,65]
- Age at time of diagnosis or transplant. Several studies have demonstrated that age at diagnosis (or at time of transplant) is a significant independent predictor of osteonecrosis.[51,52,61,57,60,63,65] Osteonecrosis is significantly more common in older children and adolescents than in younger children. In the COG-1961 trial for high-risk ALL, the 5-year cumulative incidence of symptomatic osteonecrosis was 1.0% for patients aged 1 to 9 years, 9.9% for patients aged 10 to 15 years, and 20% for patients aged 16 to 21 years (P < .0001).[51]
- Race. Osteonecrosis also occurs more frequently in whites than in blacks.[62,66]
- Genetic factors. Genetic factors influencing antifolate and glucocorticoid metabolism have also been linked to excess risk of osteonecrosis among survivors.[62] St. Jude Children's Research Hospital investigators observed an almost sixfold (odds ratio, 5.6; 95% confidence interval, 2.7-11.3) risk of osteonecrosis among survivors with polymorphism of the ACP1 gene, which regulates lipid levels and osteoblast differentiation.[56]
Studies evaluating the influence of gender on the risk of osteonecrosis have yielded conflicting results, with some suggesting a higher incidence in females [58,60,66] that has not been confirmed by others.[50,58] Osteochondroma Osteochondromas are benign boney protrusions that can be spontaneous or associated with radiation therapy. They generally occur as a single lesion, however multiple lesions may develop in the context of hereditary multiple osteochondromatosis.[67] Approximately 5% of children undergoing myeloablative stem cell transplantation will develop osteochondroma, which most commonly presents in the metaphyseal regions of long bones.[67] A large Italian study reported a 6.1% cumulative risk of developing osteochondroma at 15 years posttransplant, with increased risk associated with younger age at transplant (≤3 years) and use of TBI.[68] Osteochondromas have been reported in patients with neuroblastoma who received local radiation therapy, anti-GD2 monoclonal antibody therapy, and isotretinoin. They occurred at a median of 8.2 years from diagnosis and the cumulative incidence rate was 4.9% at 10 years from diagnosis among 362 patients younger than 10 years. In this series, most of the osteochondromas were unrelated to radiation and had features characteristic of benign developmental osteochondroma. The pathogenic role for chemotherapy, anti-GD2 monoclonal antibody therapy, or isotretinoin in the development of osteochondroma remains speculative.[69] Growth hormone therapy may influence the onset and pace of growth of osteochondromas.[17,70] Because malignant degeneration of these lesions is exceptionally rare, clinical rather than radiological follow-up is most appropriate.[71] Surgical resection is only necessary when the lesion interferes with joint alignment and movement.[72] Amputation and limb-sparing surgery Amputation and limb-sparing surgery prevent local recurrence of bone tumors by removal of all gross and microscopic disease. If optimally executed, both procedures accomplish an en bloc excision of tumor with a margin of normal uninvolved tissue. The type of surgical procedure, the primary tumor site, and the age of the patient affect the risk of postsurgical complications.[30] Complications in survivors treated with amputation include prosthetic fit problems, chronic pain in the residual limb, phantom limb pain, and bone overgrowth.[73,74] While limb-sparing surgeries may offer a more aesthetically pleasing outcome, complications have been reported more frequently in survivors who underwent these procedures than in those treated with amputation. Complications after limb-sparing surgery include non-union, pathologic fracture, aseptic loosening, limb-length discrepancy, endoprosthetic fracture, and limited joint range of motion.[73,75] Occasionally, refractory complications develop after limb-sparing surgery and require amputation.[76,77] A number of studies have compared functional outcomes after amputation and limb-sparing surgery, but results have been limited by inconsistent methods of functional assessment and small cohort sizes. Overall, data suggest that limb-sparing surgery results in better function than amputation, but differences are relatively modest.[73,77] Similarly, long-term quality of life outcomes among survivors undergoing amputation and limb sparing procedures have not differed substantially.[76] A longitudinal analysis of health status among extremity sarcoma survivors in the CCSS indicates an association between lower extremity amputation and increasing activity limitations with age, and an association between upper extremity amputation and lower educational attainment.[78] Joint contractures HCT with any history of chronic GVHD is associated with joint contractures.[79,80,81] Table 13. Bone and Joint Late Effectsa| Predisposing Therapy | Musculoskeletal Effects | Health Screening |
|---|
| CT = computed tomography; DXA = dual-energy x-ray absorptiometry; GVHD = graft-versus-host disease; HSCT = hematopoietic stem cell transplantation. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Radiation impacting musculoskeletal system | Hypoplasia; fibrosis; reduced/uneven growth (scoliosis, kyphosis); limb length discrepancy | Exam: bones and soft tissues in radiation fields | | Radiation impacting head and neck | Craniofacial abnormalities | History: psychosocial assessment, with attention to: educational and/or vocational progress, depression, anxiety, posttraumatic stress, social withdrawal | | Head and neck exam | | Radiation impacting musculoskeletal system | Radiation-induced fracture | Exam of affected bone | | Methotrexate; corticosteroids (dexamethasone, prednisone); radiation impacting skeletal structures; HSCT | Reduced bone mineral density | Bone mineral density test (DXA or quantitative CT) | | Corticosteroids (dexamethasone, prednisone) | Osteonecrosis | History: joint pain, swelling, immobility, limited range of motion | | Musculoskeletal exam | | Radiation with impact to oral cavity | Osteoradionecrosis | History/oral exam: impaired or delayed healing after dental work, persistent jaw pain or swelling, trismus | | Amputation | Amputation-related complications (impaired cosmesis, functional/activity limitations, residual limb integrity, chronic pain, increased energy expenditure) | History: pain, functional/activity limitations | | Exam: residual limb integrity | | Prosthetic evaluation | | Limb-sparing surgery | Limb-sparing surgical complications (functional/activity limitations, fibrosis, contractures, chronic infection, chronic pain, limb length discrepancy, increased energy expenditure, prosthetic malfunction [loosening, non-union, fracture]) | History: pain, functional/activity limitations | | Exam: residual limb integrity | | Radiograph of affected limb | | Orthopedic evaluation | | HSCT with any history of chronic GVHD | Joint contracture | Musculoskeletal exam | Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for musculoskeletal system late effects information, including risk factors, evaluation, and health counseling. References:
-
Green DM: 11th International Conference on Long-Term Complications of Treatment of Children and Adolescents for Cancer. Forward. Pediatr Blood Cancer 58 (1): 111, 2012.
-
Hudson MM, Neglia JP, Woods WG, et al.: Lessons from the past: opportunities to improve childhood cancer survivor care through outcomes investigations of historical therapeutic approaches for pediatric hematological malignancies. Pediatr Blood Cancer 58 (3): 334-43, 2012.
-
Estilo CL, Huryn JM, Kraus DH, et al.: Effects of therapy on dentofacial development in long-term survivors of head and neck rhabdomyosarcoma: the memorial sloan-kettering cancer center experience. J Pediatr Hematol Oncol 25 (3): 215-22, 2003.
-
Gevorgyan A, La Scala GC, Neligan PC, et al.: Radiation-induced craniofacial bone growth disturbances. J Craniofac Surg 18 (5): 1001-7, 2007.
-
Karsila-Tenovuo S, Jahnukainen K, Peltomäki T, et al.: Disturbances in craniofacial morphology in children treated for solid tumors. Oral Oncol 37 (7): 586-92, 2001.
-
Paulino AC, Simon JH, Zhen W, et al.: Long-term effects in children treated with radiotherapy for head and neck rhabdomyosarcoma. Int J Radiat Oncol Biol Phys 48 (5): 1489-95, 2000.
-
Choi SY, Kim MS, Yoo S, et al.: Long term follow-up results of external beam radiotherapy as primary treatment for retinoblastoma. J Korean Med Sci 25 (4): 546-51, 2010.
-
Sklar CA, Constine LS: Chronic neuroendocrinological sequelae of radiation therapy. Int J Radiat Oncol Biol Phys 31 (5): 1113-21, 1995.
-
Brownstein CM, Mertens AC, Mitby PA, et al.: Factors that affect final height and change in height standard deviation scores in survivors of childhood cancer treated with growth hormone: a report from the childhood cancer survivor study. J Clin Endocrinol Metab 89 (9): 4422-7, 2004.
-
Packer RJ, Boyett JM, Janss AJ, et al.: Growth hormone replacement therapy in children with medulloblastoma: use and effect on tumor control. J Clin Oncol 19 (2): 480-7, 2001.
-
Chow EJ, Friedman DL, Yasui Y, et al.: Decreased adult height in survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. J Pediatr 150 (4): 370-5, 375.e1, 2007.
-
Sklar C, Mertens A, Walter A, et al.: Final height after treatment for childhood acute lymphoblastic leukemia: comparison of no cranial irradiation with 1800 and 2400 centigrays of cranial irradiation. J Pediatr 123 (1): 59-64, 1993.
-
Bongers ME, Francken AB, Rouwé C, et al.: Reduction of adult height in childhood acute lymphoblastic leukemia survivors after prophylactic cranial irradiation. Pediatr Blood Cancer 45 (2): 139-43, 2005.
-
Huma Z, Boulad F, Black P, et al.: Growth in children after bone marrow transplantation for acute leukemia. Blood 86 (2): 819-24, 1995.
-
Leung W, Ahn H, Rose SR, et al.: A prospective cohort study of late sequelae of pediatric allogeneic hematopoietic stem cell transplantation. Medicine (Baltimore) 86 (4): 215-24, 2007.
-
Sanders JE: Growth and development after hematopoietic cell transplant in children. Bone Marrow Transplant 41 (2): 223-7, 2008.
-
Sanders JE, Guthrie KA, Hoffmeister PA, et al.: Final adult height of patients who received hematopoietic cell transplantation in childhood. Blood 105 (3): 1348-54, 2005.
-
Fletcher BD: Effects of pediatric cancer therapy on the musculoskeletal system. Pediatr Radiol 27 (8): 623-36, 1997.
-
Hogeboom CJ, Grosser SC, Guthrie KA, et al.: Stature loss following treatment for Wilms tumor. Med Pediatr Oncol 36 (2): 295-304, 2001.
-
Merchant TE, Nguyen L, Nguyen D, et al.: Differential attenuation of clavicle growth after asymmetric mantle radiotherapy. Int J Radiat Oncol Biol Phys 59 (2): 556-61, 2004.
-
Willman KY, Cox RS, Donaldson SS: Radiation induced height impairment in pediatric Hodgkin's disease. Int J Radiat Oncol Biol Phys 28 (1): 85-92, 1994.
-
Wallace WH, Shalet SM, Morris-Jones PH, et al.: Effect of abdominal irradiation on growth in boys treated for a Wilms' tumor. Med Pediatr Oncol 18 (6): 441-6, 1990.
-
Silber JH, Littman PS, Meadows AT: Stature loss following skeletal irradiation for childhood cancer. J Clin Oncol 8 (2): 304-12, 1990.
-
Hartley KA, Li C, Laningham FH, et al.: Vertebral body growth after craniospinal irradiation. Int J Radiat Oncol Biol Phys 70 (5): 1343-9, 2008.
-
Paulino AC, Wen BC, Brown CK, et al.: Late effects in children treated with radiation therapy for Wilms' tumor. Int J Radiat Oncol Biol Phys 46 (5): 1239-46, 2000.
-
Wasilewski-Masker K, Kaste SC, Hudson MM, et al.: Bone mineral density deficits in survivors of childhood cancer: long-term follow-up guidelines and review of the literature. Pediatrics 121 (3): e705-13, 2008.
-
Davies JH, Evans BA, Jenney ME, et al.: Skeletal morbidity in childhood acute lymphoblastic leukaemia. Clin Endocrinol (Oxf) 63 (1): 1-9, 2005.
-
van der Sluis IM, Boot AM, Hop WC, et al.: Long-term effects of growth hormone therapy on bone mineral density, body composition, and serum lipid levels in growth hormone deficient children: a 6-year follow-up study. Horm Res 58 (5): 207-14, 2002.
-
van der Sluis IM, van den Heuvel-Eibrink MM, Hählen K, et al.: Bone mineral density, body composition, and height in long-term survivors of acute lymphoblastic leukemia in childhood. Med Pediatr Oncol 35 (4): 415-20, 2000.
-
Oeffinger KC, Hudson MM, Landier W: Survivorship: childhood cancer survivors. Prim Care 36 (4): 743-80, 2009.
-
van der Sluis IM, van den Heuvel-Eibrink MM, Hählen K, et al.: Altered bone mineral density and body composition, and increased fracture risk in childhood acute lymphoblastic leukemia. J Pediatr 141 (2): 204-10, 2002.
-
Arikoski P, Komulainen J, Riikonen P, et al.: Reduced bone density at completion of chemotherapy for a malignancy. Arch Dis Child 80 (2): 143-8, 1999.
-
Brennan BM, Mughal Z, Roberts SA, et al.: Bone mineral density in childhood survivors of acute lymphoblastic leukemia treated without cranial irradiation. J Clin Endocrinol Metab 90 (2): 689-94, 2005.
-
Kadan-Lottick N, Marshall JA, Barón AE, et al.: Normal bone mineral density after treatment for childhood acute lymphoblastic leukemia diagnosed between 1991 and 1998. J Pediatr 138 (6): 898-904, 2001.
-
Kaste SC, Jones-Wallace D, Rose SR, et al.: Bone mineral decrements in survivors of childhood acute lymphoblastic leukemia: frequency of occurrence and risk factors for their development. Leukemia 15 (5): 728-34, 2001.
-
Warner JT, Evans WD, Webb DK, et al.: Relative osteopenia after treatment for acute lymphoblastic leukemia. Pediatr Res 45 (4 Pt 1): 544-51, 1999.
-
Mandel K, Atkinson S, Barr RD, et al.: Skeletal morbidity in childhood acute lymphoblastic leukemia. J Clin Oncol 22 (7): 1215-21, 2004.
-
Holzer G, Krepler P, Koschat MA, et al.: Bone mineral density in long-term survivors of highly malignant osteosarcoma. J Bone Joint Surg Br 85 (2): 231-7, 2003.
-
Gurney JG, Kaste SC, Liu W, et al.: Bone mineral density among long-term survivors of childhood acute lymphoblastic leukemia: results from the St. Jude Lifetime Cohort Study. Pediatr Blood Cancer 61 (7): 1270-6, 2014.
-
den Hoed MA, Klap BC, te Winkel ML, et al.: Bone mineral density after childhood cancer in 346 long-term adult survivors of childhood cancer. Osteoporos Int 26 (2): 521-9, 2015.
-
Wilson CL, Chemaitilly W, Jones KE, et al.: Modifiable Factors Associated With Aging Phenotypes Among Adult Survivors of Childhood Acute Lymphoblastic Leukemia. J Clin Oncol 34 (21): 2509-15, 2016.
-
Benmiloud S, Steffens M, Beauloye V, et al.: Long-term effects on bone mineral density of different therapeutic schemes for acute lymphoblastic leukemia or non-Hodgkin lymphoma during childhood. Horm Res Paediatr 74 (4): 241-50, 2010.
-
McClune BL, Polgreen LE, Burmeister LA, et al.: Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant 46 (1): 1-9, 2011.
-
Le Meignen M, Auquier P, Barlogis V, et al.: Bone mineral density in adult survivors of childhood acute leukemia: impact of hematopoietic stem cell transplantation and other treatment modalities. Blood 118 (6): 1481-9, 2011.
-
Kodama M, Komura H, Shimizu S, et al.: Efficacy of hormone therapy for osteoporosis in adolescent girls after hematopoietic stem cell transplantation: a longitudinal study. Fertil Steril 95 (2): 731-5, 2011.
-
Wilson CL, Dilley K, Ness KK, et al.: Fractures among long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer 118 (23): 5920-8, 2012.
-
Paulino AC: Late effects of radiotherapy for pediatric extremity sarcomas. Int J Radiat Oncol Biol Phys 60 (1): 265-74, 2004.
-
Wagner LM, Neel MD, Pappo AS, et al.: Fractures in pediatric Ewing sarcoma. J Pediatr Hematol Oncol 23 (9): 568-71, 2001.
-
Sala A, Mattano LA Jr, Barr RD: Osteonecrosis in children and adolescents with cancer - an adverse effect of systemic therapy. Eur J Cancer 43 (4): 683-9, 2007.
-
Elmantaser M, Stewart G, Young D, et al.: Skeletal morbidity in children receiving chemotherapy for acute lymphoblastic leukaemia. Arch Dis Child 95 (10): 805-9, 2010.
-
Mattano LA Jr, Devidas M, Nachman JB, et al.: Effect of alternate-week versus continuous dexamethasone scheduling on the risk of osteonecrosis in paediatric patients with acute lymphoblastic leukaemia: results from the CCG-1961 randomised cohort trial. Lancet Oncol 13 (9): 906-15, 2012.
-
Bürger B, Beier R, Zimmermann M, et al.: Osteonecrosis: a treatment related toxicity in childhood acute lymphoblastic leukemia (ALL)--experiences from trial ALL-BFM 95. Pediatr Blood Cancer 44 (3): 220-5, 2005.
-
Karimova EJ, Rai SN, Howard SC, et al.: Femoral head osteonecrosis in pediatric and young adult patients with leukemia or lymphoma. J Clin Oncol 25 (12): 1525-31, 2007.
-
Karimova EJ, Wozniak A, Wu J, et al.: How does osteonecrosis about the knee progress in young patients with leukemia?: a 2- to 7-year study. Clin Orthop Relat Res 468 (9): 2454-9, 2010.
-
Campbell S, Sun CL, Kurian S, et al.: Predictors of avascular necrosis of bone in long-term survivors of hematopoietic cell transplantation. Cancer 115 (18): 4127-35, 2009.
-
Kawedia JD, Kaste SC, Pei D, et al.: Pharmacokinetic, pharmacodynamic, and pharmacogenetic determinants of osteonecrosis in children with acute lymphoblastic leukemia. Blood 117 (8): 2340-7; quiz 2556, 2011.
-
Girard P, Auquier P, Barlogis V, et al.: Symptomatic osteonecrosis in childhood leukemia survivors: prevalence, risk factors and impact on quality of life in adulthood. Haematologica 98 (7): 1089-97, 2013.
-
Aricò M, Boccalatte MF, Silvestri D, et al.: Osteonecrosis: An emerging complication of intensive chemotherapy for childhood acute lymphoblastic leukemia. Haematologica 88 (7): 747-53, 2003.
-
Ribeiro RC, Fletcher BD, Kennedy W, et al.: Magnetic resonance imaging detection of avascular necrosis of the bone in children receiving intensive prednisone therapy for acute lymphoblastic leukemia or non-Hodgkin lymphoma. Leukemia 15 (6): 891-7, 2001.
-
te Winkel ML, Pieters R, Hop WC, et al.: Prospective study on incidence, risk factors, and long-term outcome of osteonecrosis in pediatric acute lymphoblastic leukemia. J Clin Oncol 29 (31): 4143-50, 2011.
-
Faraci M, Calevo MG, Lanino E, et al.: Osteonecrosis after allogeneic stem cell transplantation in childhood. A case-control study in Italy. Haematologica 91 (8): 1096-9, 2006.
-
Relling MV, Yang W, Das S, et al.: Pharmacogenetic risk factors for osteonecrosis of the hip among children with leukemia. J Clin Oncol 22 (19): 3930-6, 2004.
-
Vrooman LM, Stevenson KE, Supko JG, et al.: Postinduction dexamethasone and individualized dosing of Escherichia Coli L-asparaginase each improve outcome of children and adolescents with newly diagnosed acute lymphoblastic leukemia: results from a randomized study--Dana-Farber Cancer Institute ALL Consortium Protocol 00-01. J Clin Oncol 31 (9): 1202-10, 2013.
-
Yang L, Panetta JC, Cai X, et al.: Asparaginase may influence dexamethasone pharmacokinetics in acute lymphoblastic leukemia. J Clin Oncol 26 (12): 1932-9, 2008.
-
Li X, Brazauskas R, Wang Z, et al.: Avascular necrosis of bone after allogeneic hematopoietic cell transplantation in children and adolescents. Biol Blood Marrow Transplant 20 (4): 587-92, 2014.
-
Mattano LA Jr, Sather HN, Trigg ME, et al.: Osteonecrosis as a complication of treating acute lymphoblastic leukemia in children: a report from the Children's Cancer Group. J Clin Oncol 18 (18): 3262-72, 2000.
-
Bovée JV: Multiple osteochondromas. Orphanet J Rare Dis 3: 3, 2008.
-
Faraci M, Bagnasco F, Corti P, et al.: Osteochondroma after hematopoietic stem cell transplantation in childhood. An Italian study on behalf of the AIEOP-HSCT group. Biol Blood Marrow Transplant 15 (10): 1271-6, 2009.
-
Kushner BH, Roberts SS, Friedman DN, et al.: Osteochondroma in long-term survivors of high-risk neuroblastoma. Cancer 121 (12): 2090-6, 2015.
-
Bordigoni P, Turello R, Clement L, et al.: Osteochondroma after pediatric hematopoietic stem cell transplantation: report of eight cases. Bone Marrow Transplant 29 (7): 611-4, 2002.
-
Taitz J, Cohn RJ, White L, et al.: Osteochondroma after total body irradiation: an age-related complication. Pediatr Blood Cancer 42 (3): 225-9, 2004.
-
King EA, Hanauer DA, Choi SW, et al.: Osteochondromas after radiation for pediatric malignancies: a role for expanded counseling for skeletal side effects. J Pediatr Orthop 34 (3): 331-5, 2014 Apr-May.
-
Nagarajan R, Neglia JP, Clohisy DR, et al.: Limb salvage and amputation in survivors of pediatric lower-extremity bone tumors: what are the long-term implications? J Clin Oncol 20 (22): 4493-501, 2002.
-
Aulivola B, Hile CN, Hamdan AD, et al.: Major lower extremity amputation: outcome of a modern series. Arch Surg 139 (4): 395-9; discussion 399, 2004.
-
Kaste SC, Neel MN, Rao BN, et al.: Complications of limb-sparing procedures using endoprosthetic replacements about the knee for pediatric skeletal sarcomas. Pediatr Radiol 31 (2): 62-71, 2001.
-
Eiser C, Darlington AS, Stride CB, et al.: Quality of life implications as a consequence of surgery: limb salvage, primary and secondary amputation. Sarcoma 5 (4): 189-95, 2001.
-
Renard AJ, Veth RP, Schreuder HW, et al.: Function and complications after ablative and limb-salvage therapy in lower extremity sarcoma of bone. J Surg Oncol 73 (4): 198-205, 2000.
-
Marina N, Hudson MM, Jones KE, et al.: Changes in health status among aging survivors of pediatric upper and lower extremity sarcoma: a report from the childhood cancer survivor study. Arch Phys Med Rehabil 94 (6): 1062-73, 2013.
-
Antin JH: Clinical practice. Long-term care after hematopoietic-cell transplantation in adults. N Engl J Med 347 (1): 36-42, 2002.
-
Beredjiklian PK, Drummond DS, Dormans JP, et al.: Orthopaedic manifestations of chronic graft-versus-host disease. J Pediatr Orthop 18 (5): 572-5, 1998 Sep-Oct.
-
Inamoto Y, Storer BE, Petersdorf EW, et al.: Incidence, risk factors, and outcomes of sclerosis in patients with chronic graft-versus-host disease. Blood 121 (25): 5098-103, 2013.
Late Effects of the Reproductive SystemSurgery, radiation therapy, or chemotherapy that negatively affects any component of the hypothalamic-pituitary axis or gonads may compromise reproductive outcomes in childhood cancer survivors. Evidence for this outcome in childhood cancer survivors is limited by studies characterized by small sample size, cohort selection and participation bias, cross-sectional assessment, heterogeneity in treatment approach, time since treatment, and method of ascertainment. In particular, the literature is deficient regarding hard outcomes of reproductive potential (e.g., semen analysis in men, primordial follicle count in women) and outcomes after contemporary risk-adapted treatment approaches. The risk of infertility is generally related to the tissues or organs involved by the cancer and the specific type, dose, and combination of cytotoxic therapy. - Orchiectomy or oophorectomy performed for the management of pediatric germ cell tumors may reduce germ cell numbers.
- Alkylating agents and similar DNA interstrand cross-linking agents are the primary chemotherapeutic agents used in the treatment of pediatric cancers that are associated with a high risk of infertility. Factors influencing the risk of gonadal injury in children treated with alkylating agent chemotherapy include the following:
- Cumulative dose.
- The specific alkylating agent.
- The length of treatment.
- Age at treatment.
- Gender.
- The risk of radiation injury to the hypothalamic-pituitary axis or gonads is related to the treatment volume, total dose, fractionation schedule, and age at treatment.
In addition to anticancer therapy, age at treatment, and gender, it is likely that genetic factors influence the risk of permanent infertility. It should be noted that pediatric cancer treatment protocols often prescribe combined-modality therapy; thus, the additive effects of gonadotoxic exposures may need to be considered in assessing reproductive potential. Detailed information about the specific cancer treatment modalities including specific surgical procedures, the type and cumulative doses of chemotherapeutic agents, and radiation treatment volumes and doses are needed to estimate risks for gonadal dysfunction and infertility. Testis Cancer treatments that may impair testicular and reproductive function include the following: - Surgery (orchiectomy, retroperitoneal lymph node dissection, extensive pelvic dissection).
- Radiation therapy (exposing the hypothalamic-pituitary axis or testes).
- Chemotherapy (alkylating agents and similar DNA interstrand cross-linking agents such as procarbazine).
- Hematopoietic stem cell transplantation (HSCT).
Surgery affecting testicular function Patients who undergo unilateral orchiectomy for testicular torsion may have subnormal sperm counts at long-term follow-up.[1,2] Retrograde ejaculation is a frequent complication of bilateral retroperitoneal lymph node dissection performed on males with testicular neoplasms,[3,4] and impotence may occur after extensive pelvic dissections to remove a rhabdomyosarcoma of the prostate.[5] Radiation affecting testicular function Among men treated for childhood cancer, the potential for gonadal injury exists if radiation treatment fields include the pelvis, gonads, or total body. The germinal epithelium is more sensitive to radiation injury than are the androgen-producing Leydig cells. A decrease in sperm counts can be seen 3 to 6 weeks after irradiation, and depending on the dosage, recovery may take 1 to 3 years. The germinal epithelium is damaged by much lower dosages (<1 Gy) of radiation than are Leydig cells (20-30 Gy). Irreversible germ cell failure may occur with fractionated radiation doses of greater than 2 Gy to 4 Gy.[6] Administration of higher radiation doses, such as 24 Gy, which was used for the treatment of testicular relapse of acute lymphoblastic leukemia (ALL), results in both germ cell failure and Leydig cell dysfunction.[7] Radiation injury to Leydig cells is related to the dose delivered and age at treatment. Testosterone production may be normal in prepubertal boys treated with less than 12 Gy fractionated testicular irradiation, but elevated plasma concentrations of luteinizing hormone observed in this group suggest subclinical injury. Gonadal failure typically results when prepubertal boys are treated with more than 20 Gy of radiation to the testes; androgen therapy is required for masculinization. Leydig cell function is usually preserved in sexually mature male patients if radiation doses do not exceed 30 Gy. Although available data suggest that Leydig cells are more vulnerable when exposed to radiation before puberty, confounding factors, such as the age at testing and the effects of both orchiectomy and chemotherapy, limit the reliability of this observation.[8] Chemotherapy affecting testicular function Cumulative alkylating agent (e.g., cyclophosphamide, mechlorethamine, dacarbazine) dose is an important factor in estimating the risk of testicular germ cell injury, but limited studies are available that correlate results of semen analyses in clinically well-characterized cohorts.[9] In general, Leydig cell function is preserved, but germ cell failure is common in men treated with high cumulative doses of cyclophosphamide (7,500 mg/m2 or more) and more than 3 months of combination alkylating agent therapy. Most studies suggest that prepubertal males are not at lower risk for chemotherapy-induced testicular damage than are postpubertal patients.[10,11,12,13] Studies of testicular germ cell injury, as evidenced by oligospermia or azoospermia, after alkylating agent administration with or without radiation therapy, have reported the following: - Cyclophosphamide:
- Male survivors of non-Hodgkin lymphoma who received a cumulative cyclophosphamide dose of greater than 9.5 g/m2 and underwent pelvic radiation therapy were at increased risk for failure to recover spermatogenesis.[14]
- In survivors of Ewing sarcoma and soft tissue sarcoma, treatment with a cumulative cyclophosphamide dose of greater than 7.5 g/m2 was correlated with persistent oligospermia or azoospermia.[15]
- Cyclophosphamide doses exceeding 7.5 g/m2 and ifosfamide doses exceeding 60 g/m2 produced oligospermia or azoospermia in most exposed individuals.[16,17,18]
- A small cohort study reported normal semen quality in adult long-term survivors of childhood ALL treated with 0 to 10 g/m2 of cyclophosphamide and cranial irradiation, whereas no spermatozoa were detected in semen samples from survivors treated with more than 20 g/m2 of cyclophosphamide.[19]
- Treatment with a cyclophosphamide equivalent dose of less than 4 g/m2 results in infrequent azoospermia or oligospermia, with 88.6% of 31 men treated being normospermic.[20]
- Spermatogenesis was present in 67% of 15 men who received 200 mg/kg of cyclophosphamide before undergoing HSCT for aplastic anemia.[21]
- Dacarbazine:
- The combination of doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) produced oligospermia or azoospermia in adults frequently during the course of treatment. However, recovery of spermatogenesis occurred after treatment was completed, in contrast to the experience reported after treatment with mechlorethamine, vincristine, procarbazine, and prednisone (MOPP).[22]
- Alkylating agent plus procarbazine:
- Most studies suggest that combination chemotherapy with an alkylating agent and procarbazine causes severe damage to the testicular germinal epithelium that is irreversible at high cumulative doses.[10,23,24,25,26]
- Azoospermia occurred less frequently in adults after treatment with two, rather than six, cycles of MOPP.[27]
- Elevation of the basal follicle-stimulating hormone (FSH) level, reflecting impaired spermatogenesis, was less frequent among patients receiving two courses of vincristine, procarbazine, prednisone, and doxorubicin (OPPA) than among those who received two courses of OPPA in combination with two or more courses of cyclophosphamide, vincristine, procarbazine and prednisone (COPP).[28]
Testicular function after HSCT The risk of gonadal dysfunction and infertility related to conditioning with total-body irradiation (TBI), high-dose alkylating agent chemotherapy, or both is substantial. Because transplantation is often undertaken for relapsed or refractory cancer, previous treatment with alkylating agent chemotherapy or hypothalamic-pituitary axis or gonadal radiation therapy may confer additional risks. Age at treatment also influences the risk of gonadal injury. Young boys and adolescents treated with high-dose cyclophosphamide (200 mg/kg) will generally maintain Leydig cell function and testosterone production, but germ cell failure is common. After TBI conditioning, most male patients retain their ability to produce testosterone but will experience germ cell failure.[29] Limited data suggest that a greater proportion of boys will retain germinal function or recovery of spermatogenesis (based on pubertal progress and gonadotropin levels) after reduced-intensity conditioning with fludarabine/melphalan than will those treated with myeloablative conditioning with busulfan/cyclophosphamide.[30] Recovery of gonadal function Recovery of gonadal function after cytotoxic chemotherapy and radiation therapy is possible. Dutch investigators used inhibin B as a surrogate marker of gonadal function in a cross-sectional, retrospective study of 201 male survivors of childhood cancer, with a median follow-up of 15.7 years (range, 3-37 years) from diagnosis. The median inhibin B level among the cohort increased based on serial measurements performed over a median of 3.3 years (range, 0.7-11.3 years). The probability of recovery of the serum inhibin B level was significantly influenced by baseline inhibin B level, but not age at diagnosis, age at study evaluation, interval between discontinuation of treatment and study evaluation, gonadal irradiation, and alkylating agent dose score. These results suggest that recovery can occur but not if inhibin B is already at a critically low level.[31] Inhibin B and FSH levels are correlated with sperm concentration and often used to estimate the presence of spermatogenesis; however, limitations in the specificity and positive predictive value of these tests have been reported.[32] Hence, male survivors should be advised that semen analysis is the most accurate assessment of adequacy of spermatogenesis. Ovary Cancer treatments that may impair ovarian function/reserve include the following: - Surgery (oophorectomy).
- Radiation therapy (exposing the hypothalamic-pituitary axis or ovaries).
- Chemotherapy (alkylating agents, similar DNA interstrand cross-linking agents like procarbazine).
- HSCT.
Surgery affecting ovarian function Oophorectomy performed for the management of germ cell tumors may reduce ovarian reserve. Contemporary treatments utilize fertility-sparing surgical procedures combined with systemic chemotherapy to reduce this risk.[33] Radiation affecting ovarian function In women treated for childhood cancer, the potential for primary gonadal injury exists if treatment fields involve the lumbosacral spine, abdomen, pelvis, or total body. The frequency of ovarian failure after abdominal radiation therapy is related to both the age of the woman at the time of irradiation and the radiation therapy dose received by the ovaries. The ovaries of younger individuals are more resistant to radiation damage than are those of older women because of their greater complement of primordial follicles. Whole-abdomen irradiation at doses of 20 Gy or greater is associated with the highest risk of ovarian dysfunction. Seventy-one percent of women in one series failed to enter puberty, and 26% had premature menopause after receiving whole-abdominal radiation therapy doses of 20 Gy to 30 Gy.[34] Other studies reported similar results in women treated with whole-abdomen irradiation [35] or craniospinal irradiation [36,37] during childhood. Chemotherapy affecting ovarian function Ovarian function may be impaired after treatment with combination chemotherapy that includes an alkylating agent and procarbazine. In general, girls maintain gonadal function at higher cumulative alkylating agent doses than do boys. Most female childhood cancer survivors who are treated with risk-adapted combination chemotherapy retain or recover ovarian function. However, the risk of acute ovarian failure and premature menopause is substantial if treatment includes combined-modality therapy with alkylating agent chemotherapy and abdominal or pelvic radiation therapy or dose-intensive alkylating agents for myeloablative conditioning before HSCT.[38,39,40,41] Premature ovarian failure Premature ovarian failure is well documented in childhood cancer survivors, especially in women treated with both an alkylating agent and abdominal radiation therapy.[38,42,43] Studies have associated the following factors with an increased rate of premature ovarian failure (acute ovarian failure and premature menopause): - Age at the time of treatment and attained age.
- Increasing doses of abdominal-pelvic radiation therapy.
- Exposure to alkylating agents and/or procarbazine.
- Oophorectomy.
The presence of apparently normal ovarian function at the completion of chemotherapy should not be interpreted as evidence that no ovarian injury has occurred. Studies of acute ovarian failure and premature menopause have observed the following: - Of 3,390 eligible participants in the Childhood Cancer Survivor Study (CCSS), 215 (6.3%) developed acute ovarian failure (defined as never having menses or ceased having menses within 5 years of diagnosis). Survivors with acute ovarian failure were older (aged 13-20 years vs. aged 0-12 years) at cancer diagnosis and more likely to have been diagnosed with Hodgkin lymphoma or to have received abdominal or pelvic radiation therapy than were survivors without acute ovarian failure.[39] Of survivors who developed acute ovarian failure, 75% had received abdominal-pelvic radiation therapy. Radiation doses to the ovary of at least 20 Gy were associated with the highest rate of acute ovarian failure, with over 70% of such patients developing acute ovarian failure. In a multivariable logistic regression model, increasing doses of ovarian radiation, exposure to procarbazine at any age, and exposure to cyclophosphamide at ages 13 to 20 years were independent risk factors for acute ovarian failure.[39]
- A total of 126 childhood cancer survivors and 33 control siblings who participated in the CCSS developed premature menopause, defined as cessation of menses before 40 years. The cumulative incidence of nonsurgical premature menopause was substantially higher for survivors than for siblings (8% vs. 0.8%; relative risk [RR], 13.21; 95% confidence interval [CI], 3.26-53.51; P < .001) (refer to Figure 9).[38] A multiple Poisson regression model showed that risk factors for nonsurgical premature menopause included attained age, exposure to increasing doses of radiation to the ovaries, increasing alkylating agent dose score, and a diagnosis of Hodgkin lymphoma. For survivors who were treated with alkylating agents plus abdominal-pelvic radiation therapy, the cumulative incidence of nonsurgical premature menopause approached 30%.[38]
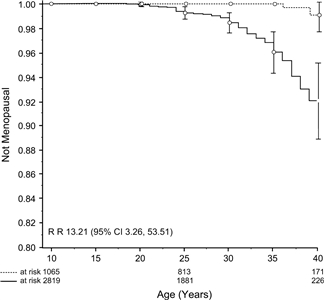
Figure 9. Cumulative incidence curves of nonsurgical premature menopause in survivors (solid line) compared with siblings (broken line). Vertical bars indicate 95% confidence intervals. Sklar C A et al. JNCI J Natl Cancer Inst 2006;98:890-896. ©Sklar 2006. Published by Oxford University Press. - A French cohort study of 1,109 female survivors of childhood solid cancer identified the following as risk factors for nonsurgical menopause:[43]
- Exposure to and dose of alkylating agents, especially during adolescence.
- Radiation dose to the ovaries.
- Oophorectomy.
Women treated with alkylating agents after the onset of puberty, either alone (RR, 9; 95% CI, 2.7-28; P = .0003) or associated with even a low dose of radiation to the ovaries (RR, 29; 95% CI, 8-108; P < .0001), had the highest risk ratio for nonsurgical menopause. Unilateral oophorectomy was associated with a 7-year-earlier age at menopause. The overall rate of nonsurgical menopause by age 40 years was only 2.1% and substantially lower than the CCSS and European Organization for Research and Treatment of Cancer cohort studies that include survivors of hematological malignancies.[43] - In Europe, survivors of Hodgkin lymphoma treated between the ages 15 years and 40 years and who were not receiving hormonal contraceptives were surveyed for the occurrence of premature ovarian failure. In 460 women, premature ovarian failure was mainly influenced by alkylating chemotherapy use with a linear dose relationship between alkylating chemotherapy and premature ovarian failure occurrence. Premature ovarian failure risk increased by 23% per year of age at treatment. In women treated without alkylating chemotherapy before age 32 years and at age 32 years or older, cumulative premature ovarian failure risks were 3% and 9%, respectively. If menstruation returned after treatment, cumulative premature ovarian failure risk was independent of age at treatment. Among women who ultimately developed premature ovarian failure, 22% had one or more children after treatment, compared with 41% of women without premature ovarian failure who had one or more children after treatment. This report indicates that women with proven fertility after treatment can still face infertility problems at a later stage.[42]
Ovarian function after HSCT The preservation of ovarian function among women treated with HSCT is related to age at treatment, receipt of pretransplant alkylating agent chemotherapy and abdominal-pelvic radiation therapy, and transplant conditioning regimen.[40,44] Studies of ovarian function among women treated with HSCT have observed the following: - Girls and young women conditioned with TBI or busulfan-based regimens appear to be at equally high risk of declining ovarian function and premature menopause compared with patients conditioned with cyclophosphamide only.[40] All women who received high-dose (50 mg/kg/day x 4 days) cyclophosphamide before HSCT for aplastic anemia developed amenorrhea after transplantation. In one series, 36 of 43 women with aplastic anemia conditioned with cyclophosphamide (200 mg/kg) had recovery of normal ovarian function 3 to 42 months after transplantation, including all of the 27 patients who were between ages 13 and 25 years at the time of HSCT.[41]
- TBI is especially damaging when given in a single fraction.[40] Most postpubertal women who receive TBI before HSCT develop amenorrhea. In one series, recovery of normal ovarian function occurred in only 9 of 144 patients and was highly correlated with age at time of radiation therapy in patients younger than 25 years.[41]
- Among women with leukemia, cranial irradiation before transplantation further decreased the possibility of retaining ovarian function.[40]
- Ovarian function may be better preserved (based on pubertal progress and gonadotropin levels) in females undergoing HSCT with reduced-intensity conditioning using fludarabine/melphalan than in those undergoing conditioning with myeloablative busulfan/cyclophosphamide.[30]
Fertility Infertility remains one of the most common life-altering treatment effects experienced by long-term childhood survivors. Pediatric cancer cohort studies demonstrate the impact of cytotoxic therapy on reproductive outcomes. CCSS investigations have elucidated factors contributing to subfertility among childhood cancer survivors. Fertility was evaluated in 10,938 CCSS participants (5,640 males, 5,298 females) and 3,949 siblings.[45] - At a median follow-up of 8 years from cohort entry, 38% of survivors reported having or siring a pregnancy, resulting in at least one live birth in 83% of those survivors. Among siblings monitored for a median of 10 years, 62% reported having or siring a pregnancy, resulting in at least one live birth in 90% of those siblings. Multivariable analysis confirmed that survivors had significantly decreased likelihood of siring or having a pregnancy (hazard ratio [HR], 0.63 in males and 0.87 in females) or of having a live birth (HR, 0.63 in males and 0.82 in females) than did siblings.
- Greater doses of alkylating drugs (HR, 0.82 per 5,000 mg/m2 increments) and cisplatin reduced the likelihood of siring pregnancy among male survivors, but only busulfan and higher doses (>411 mg/m2) of lomustine significantly reduced pregnancy among females. Reassuringly, the risk of reduced likelihood of pregnancy in women was observed only at the highest cyclophosphamide equivalent dose (HR, 0.85 for upper quartile [≥11,295 mg/m2] vs. no exposure).
- HRs (95% CIs) for the likelihood of reporting first pregnancy by cyclophosphamide equivalent dose for male and female survivors are summarized in Table 14:
Table 14. Cyclophosphamide Equivalent Dose by Tertile and Gender| Cyclophosphamide Equivalent Dose by Tertile | Male | Female |
|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value |
|---|
| CI = confidence interval; HR = hazard ratio. | | Lower (<4,897 mg/m2) | 1.14 (1.00-1.30) | .045 | 0.97 (0.86-1.08) | .55 | | Middle (4,897-9,638 mg/m2) | 0.79 (0.68-0.91) | .0010 | 0.98 (0.87-1.11) | .76 | | Upper (≥9,639 mg/m2) | 0.55 (0.47-0.64) | <.0001 | 0.90 (0.79-1.01) | .07 | - Similar relationships were observed for live birth outcomes.
Fertility may be impaired by factors other than the absence of sperm and ova. Conception requires delivery of sperm to the uterine cervix, patency of the fallopian tubes for fertilization to occur, and appropriate conditions in the uterus for implantation. [3,4,46] - Retrograde ejaculation occurs with a significant frequency in men who undergo bilateral retroperitoneal lymph node dissection.[3,4]
- Uterine structure may be affected by abdominal irradiation. A study demonstrated that uterine length was significantly shorter in ten women with ovarian failure who had been treated with whole-abdomen irradiation. Endometrial thickness did not increase in response to hormone replacement therapy in three women who underwent weekly ultrasound examination. No flow was detectable with Doppler ultrasound through either uterine artery of five women, and through one uterine artery in three additional women.[46]
Reproduction For survivors who maintain fertility, numerous investigations have evaluated the prevalence of and risk factors for pregnancy complications in adults treated for cancer during childhood. Pregnancy complications including hypertension, fetal malposition, fetal loss/spontaneous abortion, preterm labor, and low birth weight have been observed in association with specific diagnostic and treatment groups.[47,48,49,50,51,52,53,54,55,56,57] - In a study of 4,029 pregnancies among 1,915 women followed in the CCSS, there were 63% live births, 1% stillbirths, 15% miscarriages, 17% abortions, and 3% unknown or in gestation. Risk of miscarriage was 3.6-fold higher in women treated with craniospinal irradiation and 1.7-fold higher in those treated with pelvic irradiation. Chemotherapy exposure alone did not increase risk of miscarriage. Survivors were less likely to have live births, more likely to have medical abortions, and more likely to have low-birth-weight babies than were siblings.[47] Disruption of normal uterine function after radiation therapy or other treatment that results in reduced uterine volume and impaired uterine blood flow appears to be the underlying pathophysiology for many of these adverse obstetrical events.[58]
- In the National Wilms Tumor Study, records were obtained for 1,021 pregnancies of more than 20 weeks duration. In this group, there were 955 single live births. Hypertension complicating pregnancy, early or threatened labor, malposition of the fetus, lower birth weight (<2,500 g), and premature delivery (<36 weeks) were more frequent among women who had received flank irradiation, in a dose-dependent manner.[59]
- Another CCSS study evaluated pregnancy outcomes of partners of male survivors. Among 4,106 sexually active males, 1,227 reported they sired 2,323 pregnancies, which resulted in 69% live births, 13% miscarriages, 13% abortions, and 5% unknown or in gestation at the time of analysis. Compared with partners of male siblings, there was a decreased incidence of live births (RR, 0.77), but no significant differences of pregnancy outcome by treatment.[48]
- Results from a Danish study confirm the association of uterine irradiation with spontaneous abortion, but not other types of abortion. Thirty-four thousand pregnancies were evaluated in a population of 1,688 female survivors of childhood cancer in the Danish Cancer Registry. The pregnancy outcomes of survivors, 2,737 sisters, and 16,700 comparison women in the population were identified. No significant differences were seen between survivors and comparison women in the proportions of live births, stillbirths, or all types of abortions combined. Survivors with a history of neuroendocrine or abdominal radiation therapy had an increased risk of spontaneous abortion. Thus, the pregnancy outcomes of survivors were similar to those of comparison women with the exception of spontaneous abortion.[49]
- In a retrospective cohort analysis from the CCSS of 1,148 men and 1,657 women who had survived cancer, there were 4,946 pregnancies. Irradiation of the testes in men and pituitary gland in women and chemotherapy with alkylating drugs were not associated with an increased risk of stillbirth or neonatal death. Uterine and ovarian irradiation significantly increased the risk of stillbirth and neonatal death at doses higher than 10 Gy. For girls treated before menarche, irradiation of the uterus and ovaries at doses as low as 1 Gy to 2.49 Gy significantly increased the risk of stillbirth or neonatal death.[56]
- Most pregnancies reported by HSCT survivors and their partners result in live births. In female HSCT survivors who were exposed to TBI, there appears to be an increased risk of preterm delivery of low-birth-weight infants. Female HSCT survivors are at higher risk of needing Cesarean sections than are the normal population (42% vs. 16%). [57]
- Preservation of fertility and successful pregnancies may occur after HSCT, although the conditioning regimens that include TBI, cyclophosphamide, and busulfan are highly gonadotoxic. One study evaluated pregnancy outcomes in a group of females treated with HSCT. Among 708 women who were postpubertal at the time of transplant, 116 regained normal ovarian function and 32 became pregnant. Among 82 women who were prepubertal at the time of transplant, 23 had normal ovarian function and nine became pregnant. Of the 72 pregnancies in these 41 women, 16 occurred in those treated with TBI and 50% resulted in early termination. Among the 56 pregnancies in women treated with cyclophosphamide without either TBI or busulfan, 21% resulted in early termination. There were no pregnancies among the 73 women treated with busulfan and cyclophosphamide, and only one retained ovarian function.[60]
- A German study demonstrated that the rate of childbearing for female survivors of Hodgkin lymphoma was similar to that of the general population, although the rate of childbearing was lower for survivors who received pelvic radiation therapy.[61]
Fertility preservation Progress in reproductive endocrinology has resulted in the availability of several options for preserving or permitting fertility in patients about to receive potentially toxic chemotherapy or radiation therapy.[62] For males, cryopreservation of spermatozoa before treatment is an effective method to circumvent the sterilizing effect of therapy. Although pretreatment semen quality in patients with cancer has been shown to be less than that noted in healthy donors, the percentage decline in semen quality and the effect of cryodamage to spermatozoa from patients with cancer is similar to that of normal donors.[63,64] For those unable to bank sperm, newer technologies such as testicular sperm extraction may be an option. Further micromanipulative technologic advances such as intracytoplasmic sperm injection and similar techniques may be able to render sperm extracted surgically, or even poor-quality cryopreserved spermatozoa from cancer patients, capable of successful fertilization.[65] For females, the most successful assisted-reproductive techniques depend on harvesting and banking the postpubertal patient's oocytes and cryopreserving unfertilized oocytes or embryos before gonadotoxic therapy.[66] Options for prepubertal patients are limited to investigational ovarian tissue cryopreservation for later autotransplantation, which may be offered to girls with nonovarian, nonhematologic cancers.[67] Offspring of childhood cancer survivors For childhood cancer survivors who have offspring, there is concern about congenital anomalies, genetic disease, or risk of cancer in the offspring. Children of cancer survivors are not at significantly increased risk for congenital anomalies stemming from their parents' exposure to mutagenic cancer treatments, as supported by the following observations: - A retrospective cohort analysis of validated cases of congenital anomalies among 4,699 children of 1,128 male and 1,627 female participants of the CCSS showed no significant associations between gonadal radiation therapy or cumulative exposure to alkylating agents and congenital anomalies in offspring.[68]
- In a report of 2,198 offspring of adult survivors treated for childhood cancer between 1945 and 1975 compared with 4,544 offspring of sibling controls, there were no differences in the proportion of offspring with cytogenetic syndromes, single-gene defects, or simple malformations. There was similarly no effect of type of childhood cancer treatment on the occurrence of genetic disease in the offspring. A population-based study of 2,630 live-born offspring of childhood cancer survivors versus 5,504 live-born offspring of the survivors' siblings found no differences in proportion of abnormal karyotypes or incidence of Down syndrome or Turner syndrome between survivor and sibling offspring.[69]
- In the same population-based cohort, survivors treated with abdominal radiation therapy and/or alkylating agents did not have an increased risk of offspring with genetic disease, compared with survivors not exposed to these agents.[70]
- In a study of 5,847 offspring of survivors of childhood cancers treated in five Scandinavian countries, in the absence of a hereditary cancer syndrome (such as hereditary retinoblastoma), there was no increased risk of cancer.[71] Data from the five-center study also indicated no excess risk of single-gene disorders, congenital malformations, or chromosomal syndromes among the offspring of former patients compared with the offspring of siblings.[72]
- In a study that evaluated pregnancy outcomes in 19,412 allogeneic and 17,950 autologous transplant patients, European Group for Blood and Marrow Transplantation investigators did not observe an increased risk of birth defects, developmental delay, or cancer among offspring of male and female HSCT recipients.[57]
Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for reproductive late effects information including risk factors, evaluation, and health counseling. References:
-
Arap MA, Vicentini FC, Cocuzza M, et al.: Late hormonal levels, semen parameters, and presence of antisperm antibodies in patients treated for testicular torsion. J Androl 28 (4): 528-32, 2007 Jul-Aug.
-
Tryfonas G, Violaki A, Tsikopoulos G, et al.: Late postoperative results in males treated for testicular torsion during childhood. J Pediatr Surg 29 (4): 553-6, 1994.
-
Narayan P, Lange PH, Fraley EE: Ejaculation and fertility after extended retroperitoneal lymph node dissection for testicular cancer. J Urol 127 (4): 685-8, 1982.
-
Nijman JM, Jager S, Boer PW, et al.: The treatment of ejaculation disorders after retroperitoneal lymph node dissection. Cancer 50 (12): 2967-71, 1982.
-
Schlegel PN, Walsh PC: Neuroanatomical approach to radical cystoprostatectomy with preservation of sexual function. J Urol 138 (6): 1402-6, 1987.
-
Hahn EW, Feingold SM, Simpson L, et al.: Recovery from aspermia induced by low-dose radiation in seminoma patients. Cancer 50 (2): 337-40, 1982.
-
Blatt J, Sherins RJ, Niebrugge D, et al.: Leydig cell function in boys following treatment for testicular relapse of acute lymphoblastic leukemia. J Clin Oncol 3 (9): 1227-31, 1985.
-
Izard MA: Leydig cell function and radiation: a review of the literature. Radiother Oncol 34 (1): 1-8, 1995.
-
Romerius P, Ståhl O, Moëll C, et al.: High risk of azoospermia in men treated for childhood cancer. Int J Androl 34 (1): 69-76, 2011.
-
Shafford EA, Kingston JE, Malpas JS, et al.: Testicular function following the treatment of Hodgkin's disease in childhood. Br J Cancer 68 (6): 1199-204, 1993.
-
Whitehead E, Shalet SM, Jones PH, et al.: Gonadal function after combination chemotherapy for Hodgkin's disease in childhood. Arch Dis Child 57 (4): 287-91, 1982.
-
Aubier F, Flamant F, Brauner R, et al.: Male gonadal function after chemotherapy for solid tumors in childhood. J Clin Oncol 7 (3): 304-9, 1989.
-
Jaffe N, Sullivan MP, Ried H, et al.: Male reproductive function in long-term survivors of childhood cancer. Med Pediatr Oncol 16 (4): 241-7, 1988.
-
Pryzant RM, Meistrich ML, Wilson G, et al.: Long-term reduction in sperm count after chemotherapy with and without radiation therapy for non-Hodgkin's lymphomas. J Clin Oncol 11 (2): 239-47, 1993.
-
Meistrich ML, Wilson G, Brown BW, et al.: Impact of cyclophosphamide on long-term reduction in sperm count in men treated with combination chemotherapy for Ewing and soft tissue sarcomas. Cancer 70 (11): 2703-12, 1992.
-
Kenney LB, Laufer MR, Grant FD, et al.: High risk of infertility and long term gonadal damage in males treated with high dose cyclophosphamide for sarcoma during childhood. Cancer 91 (3): 613-21, 2001.
-
Garolla A, Pizzato C, Ferlin A, et al.: Progress in the development of childhood cancer therapy. Reprod Toxicol 22 (2): 126-32, 2006.
-
Williams D, Crofton PM, Levitt G: Does ifosfamide affect gonadal function? Pediatr Blood Cancer 50 (2): 347-51, 2008.
-
Jahnukainen K, Heikkinen R, Henriksson M, et al.: Semen quality and fertility in adult long-term survivors of childhood acute lymphoblastic leukemia. Fertil Steril 96 (4): 837-42, 2011.
-
Green DM, Liu W, Kutteh WH, et al.: Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study. Lancet Oncol 15 (11): 1215-23, 2014.
-
Sanders JE, Buckner CD, Leonard JM, et al.: Late effects on gonadal function of cyclophosphamide, total-body irradiation, and marrow transplantation. Transplantation 36 (3): 252-5, 1983.
-
Viviani S, Santoro A, Ragni G, et al.: Gonadal toxicity after combination chemotherapy for Hodgkin's disease. Comparative results of MOPP vs ABVD. Eur J Cancer Clin Oncol 21 (5): 601-5, 1985.
-
Mackie EJ, Radford M, Shalet SM: Gonadal function following chemotherapy for childhood Hodgkin's disease. Med Pediatr Oncol 27 (2): 74-8, 1996.
-
Sherins RJ, Olweny CL, Ziegler JL: Gynecomastia and gonadal dysfunction in adolescent boys treated with combination chemotherapy for Hodgkin's disease. N Engl J Med 299 (1): 12-6, 1978.
-
Dhabhar BN, Malhotra H, Joseph R, et al.: Gonadal function in prepubertal boys following treatment for Hodgkin's disease. Am J Pediatr Hematol Oncol 15 (3): 306-10, 1993.
-
Heikens J, Behrendt H, Adriaanse R, et al.: Irreversible gonadal damage in male survivors of pediatric Hodgkin's disease. Cancer 78 (9): 2020-4, 1996.
-
da Cunha MF, Meistrich ML, Fuller LM, et al.: Recovery of spermatogenesis after treatment for Hodgkin's disease: limiting dose of MOPP chemotherapy. J Clin Oncol 2 (6): 571-7, 1984.
-
Brämswig JH, Heimes U, Heiermann E, et al.: The effects of different cumulative doses of chemotherapy on testicular function. Results in 75 patients treated for Hodgkin's disease during childhood or adolescence. Cancer 65 (6): 1298-302, 1990.
-
Ishiguro H, Yasuda Y, Tomita Y, et al.: Gonadal shielding to irradiation is effective in protecting testicular growth and function in long-term survivors of bone marrow transplantation during childhood or adolescence. Bone Marrow Transplant 39 (8): 483-90, 2007.
-
Panasiuk A, Nussey S, Veys P, et al.: Gonadal function and fertility after stem cell transplantation in childhood: comparison of a reduced intensity conditioning regimen containing melphalan with a myeloablative regimen containing busulfan. Br J Haematol 170 (5): 719-26, 2015.
-
van Dorp W, van der Geest IM, Laven JS, et al.: Gonadal function recovery in very long-term male survivors of childhood cancer. Eur J Cancer 49 (6): 1280-6, 2013.
-
Green DM, Zhu L, Zhang N, et al.: Lack of specificity of plasma concentrations of inhibin B and follicle-stimulating hormone for identification of azoospermic survivors of childhood cancer: a report from the St Jude lifetime cohort study. J Clin Oncol 31 (10): 1324-8, 2013.
-
Tangir J, Zelterman D, Ma W, et al.: Reproductive function after conservative surgery and chemotherapy for malignant germ cell tumors of the ovary. Obstet Gynecol 101 (2): 251-7, 2003.
-
Wallace WH, Shalet SM, Crowne EC, et al.: Ovarian failure following abdominal irradiation in childhood: natural history and prognosis. Clin Oncol (R Coll Radiol) 1 (2): 75-9, 1989.
-
Scott JE: Pubertal development in children treated for nephroblastoma. J Pediatr Surg 16 (2): 122-5, 1981.
-
Hamre MR, Robison LL, Nesbit ME, et al.: Effects of radiation on ovarian function in long-term survivors of childhood acute lymphoblastic leukemia: a report from the Childrens Cancer Study Group. J Clin Oncol 5 (11): 1759-65, 1987.
-
Wallace WH, Shalet SM, Tetlow LJ, et al.: Ovarian function following the treatment of childhood acute lymphoblastic leukaemia. Med Pediatr Oncol 21 (5): 333-9, 1993.
-
Sklar CA, Mertens AC, Mitby P, et al.: Premature menopause in survivors of childhood cancer: a report from the childhood cancer survivor study. J Natl Cancer Inst 98 (13): 890-6, 2006.
-
Chemaitilly W, Mertens AC, Mitby P, et al.: Acute ovarian failure in the childhood cancer survivor study. J Clin Endocrinol Metab 91 (5): 1723-8, 2006.
-
Vatanen A, Wilhelmsson M, Borgström B, et al.: Ovarian function after allogeneic hematopoietic stem cell transplantation in childhood and adolescence. Eur J Endocrinol 170 (2): 211-8, 2014.
-
Sanders JE, Buckner CD, Amos D, et al.: Ovarian function following marrow transplantation for aplastic anemia or leukemia. J Clin Oncol 6 (5): 813-8, 1988.
-
van der Kaaij MA, Heutte N, Meijnders P, et al.: Premature ovarian failure and fertility in long-term survivors of Hodgkin's lymphoma: a European Organisation for Research and Treatment of Cancer Lymphoma Group and Groupe d'Etude des Lymphomes de l'Adulte Cohort Study. J Clin Oncol 30 (3): 291-9, 2012.
-
Thomas-Teinturier C, El Fayech C, Oberlin O, et al.: Age at menopause and its influencing factors in a cohort of survivors of childhood cancer: earlier but rarely premature. Hum Reprod 28 (2): 488-95, 2013.
-
Bresters D, Emons JA, Nuri N, et al.: Ovarian insufficiency and pubertal development after hematopoietic stem cell transplantation in childhood. Pediatr Blood Cancer 61 (11): 2048-53, 2014.
-
Chow EJ, Stratton KL, Leisenring WM, et al.: Pregnancy after chemotherapy in male and female survivors of childhood cancer treated between 1970 and 1999: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol 17 (5): 567-76, 2016.
-
Critchley HO, Wallace WH, Shalet SM, et al.: Abdominal irradiation in childhood; the potential for pregnancy. Br J Obstet Gynaecol 99 (5): 392-4, 1992.
-
Green DM, Kawashima T, Stovall M, et al.: Fertility of female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 27 (16): 2677-85, 2009.
-
Green DM, Kawashima T, Stovall M, et al.: Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 28 (2): 332-9, 2010.
-
Winther JF, Boice JD Jr, Svendsen AL, et al.: Spontaneous abortion in a Danish population-based cohort of childhood cancer survivors. J Clin Oncol 26 (26): 4340-6, 2008.
-
Cvancarova M, Samuelsen SO, Magelssen H, et al.: Reproduction rates after cancer treatment: experience from the Norwegian radium hospital. J Clin Oncol 27 (3): 334-43, 2009.
-
Magelssen H, Melve KK, Skjaerven R, et al.: Parenthood probability and pregnancy outcome in patients with a cancer diagnosis during adolescence and young adulthood. Hum Reprod 23 (1): 178-86, 2008.
-
Hawkins MM, Smith RA: Pregnancy outcomes in childhood cancer survivors: probable effects of abdominal irradiation. Int J Cancer 43 (3): 399-402, 1989.
-
Chow EJ, Kamineni A, Daling JR, et al.: Reproductive outcomes in male childhood cancer survivors: a linked cancer-birth registry analysis. Arch Pediatr Adolesc Med 163 (10): 887-94, 2009.
-
Mueller BA, Chow EJ, Kamineni A, et al.: Pregnancy outcomes in female childhood and adolescent cancer survivors: a linked cancer-birth registry analysis. Arch Pediatr Adolesc Med 163 (10): 879-86, 2009.
-
Reulen RC, Zeegers MP, Wallace WH, et al.: Pregnancy outcomes among adult survivors of childhood cancer in the British Childhood Cancer Survivor Study. Cancer Epidemiol Biomarkers Prev 18 (8): 2239-47, 2009.
-
Signorello LB, Mulvihill JJ, Green DM, et al.: Stillbirth and neonatal death in relation to radiation exposure before conception: a retrospective cohort study. Lancet 376 (9741): 624-30, 2010.
-
Salooja N, Szydlo RM, Socie G, et al.: Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey. Lancet 358 (9278): 271-6, 2001.
-
Beneventi F, Locatelli E, Giorgiani G, et al.: Adolescent and adult uterine volume and uterine artery Doppler blood flow among subjects treated with bone marrow transplantation or chemotherapy in pediatric age: a case-control study. Fertil Steril 103 (2): 455-61, 2015.
-
Green DM, Lange JM, Peabody EM, et al.: Pregnancy outcome after treatment for Wilms tumor: a report from the national Wilms tumor long-term follow-up study. J Clin Oncol 28 (17): 2824-30, 2010.
-
Sanders JE, Hawley J, Levy W, et al.: Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood 87 (7): 3045-52, 1996.
-
Brämswig JH, Riepenhausen M, Schellong G: Parenthood in adult female survivors treated for Hodgkin's lymphoma during childhood and adolescence: a prospective, longitudinal study. Lancet Oncol 16 (6): 667-75, 2015.
-
Loren AW, Mangu PB, Beck LN, et al.: Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31 (19): 2500-10, 2013.
-
Agarwa A: Semen banking in patients with cancer: 20-year experience. Int J Androl 23 (Suppl 2): 16-9, 2000.
-
Müller J, Sønksen J, Sommer P, et al.: Cryopreservation of semen from pubertal boys with cancer. Med Pediatr Oncol 34 (3): 191-4, 2000.
-
Hsiao W, Stahl PJ, Osterberg EC, et al.: Successful treatment of postchemotherapy azoospermia with microsurgical testicular sperm extraction: the Weill Cornell experience. J Clin Oncol 29 (12): 1607-11, 2011.
-
Domingo J, Ayllón Y, Domingo S, et al.: New approaches to female fertility preservation. Clin Transl Oncol 11 (3): 154-9, 2009.
-
Oktay K, Karlikaya G: Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med 342 (25): 1919, 2000.
-
Signorello LB, Mulvihill JJ, Green DM, et al.: Congenital anomalies in the children of cancer survivors: a report from the childhood cancer survivor study. J Clin Oncol 30 (3): 239-45, 2012.
-
Winther JF, Boice JD Jr, Mulvihill JJ, et al.: Chromosomal abnormalities among offspring of childhood-cancer survivors in Denmark: a population-based study. Am J Hum Genet 74 (6): 1282-5, 2004.
-
Winther JF, Olsen JH, Wu H, et al.: Genetic disease in the children of Danish survivors of childhood and adolescent cancer. J Clin Oncol 30 (1): 27-33, 2012.
-
Sankila R, Olsen JH, Anderson H, et al.: Risk of cancer among offspring of childhood-cancer survivors. Association of the Nordic Cancer Registries and the Nordic Society of Paediatric Haematology and Oncology. N Engl J Med 338 (19): 1339-44, 1998.
-
Byrne J, Rasmussen SA, Steinhorn SC, et al.: Genetic disease in offspring of long-term survivors of childhood and adolescent cancer. Am J Hum Genet 62 (1): 45-52, 1998.
Late Effects of the Respiratory SystemSpecific chemotherapeutic agents, thoracic radiation therapy, pulmonary/chest wall surgery, and hematopoietic stem cell transplantation (HSCT) can compromise respiratory function in long-term survivors of childhood cancer. The effects of early lung injury from cancer treatment may be exacerbated by the decline in lung function associated with normal aging, other comorbid chronic health conditions, or smoking. The quality of current evidence regarding this outcome is limited by retrospective data collection, small sample size, cohort selection and participation bias, description of outcomes following antiquated treatment approaches, and variability in time since treatment and method of ascertainment. The true prevalence or incidence of pulmonary dysfunction in childhood cancer survivors is not clear. For children treated with HSCT, there is significant clinical disease. Evidence for this outcome in childhood cancer survivors is limited by studies characterized by small sample size, cohort selection and participation bias, cross-sectional assessment, heterogeneity in treatment approach, time since treatment, and method of ascertainment. Notably, no large cohort studies have been performed with clinical evaluations coupled with functional and quality-of-life assessments. Results from selected cohort studies featuring long-term pulmonary function outcomes include the following: - An analysis of self-reported pulmonary complications of 12,390 survivors of common childhood malignancies has been reported by the Childhood Cancer Survivor Study.[1] This cohort includes children treated with both conventional and myeloablative therapies. Compared with siblings, survivors had an increased relative risk (RR) of lung fibrosis, recurrent pneumonia, chronic cough, pleurisy, use of supplemental oxygen therapy, abnormal chest wall, exercise-induced shortness of breath, and bronchitis, with RRs ranging from 1.2 to 13.0 (highest for lung fibrosis and lowest for bronchitis). The 25-year cumulative incidence of lung fibrosis was 5% for those who received chest radiation therapy and less than 1% for those who received pulmonary toxic chemotherapy.
- The incidence of self-reported pulmonary dysfunction among a subset of adults in the same cohort treated for central nervous system malignancies with craniospinal irradiation (per 1,000 person-years) was 9.1 (95% confidence interval, 7.8-10.6) for emphysema/obliterative bronchiolitis and more than 3.0 for asthma, chronic cough, and need for extra oxygen. High rates of late onset pulmonary dysfunction occurring more than 5 years after diagnosis were also observed.[2]
- Dutch investigators reported outcomes of 193 childhood cancer survivors evaluated by pulmonary function testing at a median follow-up of 18 years after diagnosis. Pulmonary function impairment (Common Terminology Criteria for Adverse Events grade 2 or higher) was identified in 85 patients (44.0%) and included obstructive deficits (2.1%), restrictive deficits (17.6%), and decreased carbon monoxide diffusion capacity (39.9%). Multivariate logistic regression models showed that, compared with bleomycin treatment only, treatment with radiation therapy, radiation therapy combined with bleomycin, and radiation therapy combined with surgery were associated with the highest risk of pulmonary function impairment.[3]
- In a longitudinal study evaluating the magnitude and trajectory of pulmonary dysfunction among 121 childhood cancer survivors (median time from diagnosis to last evaluation, 17.1 years) treated with potentially pulmonary-toxic therapy (e.g., bleomycin, busulfan, pulmonary radiation therapy), survivors were significantly more likely to have restrictive and diffusion defects than were healthy controls.[4] Age younger than 16 years at diagnosis and exposure to more than 20 Gy of chest radiation were associated with increased odds of restrictive defects, whereas female gender and chest radiation dose were associated with diffusion abnormalities. Decline in pulmonary function over time was largely related to changes in diffusion capacity. The odds of decline in diffusion function over time showed a fourfold increase among females and 24-fold increase among survivors treated with more than 20 Gy of chest radiation. Compared with survivors with normal diffusion, those with diffusion defects were significantly more likely to be symptomatic and have poorer health-related quality-of-life scores, with decreases in the domains of physical functioning, role limitation as a result of physical health, and low energy/increased fatigue.
Respiratory complications following radiation therapy Radiation therapy that exposes the lung parenchyma can result in pulmonary dysfunction related to reduced lung volume, impaired dynamic compliance, and deformity of both the lung and chest wall. The potential for chronic pulmonary sequelae is related to the radiation dose administered, the volume of lung irradiated, and the fractional radiation therapy doses.[5] Combined-modality therapy including radiation therapy and pulmonary toxic chemotherapy or thoracic/chest wall surgery increases the risk of pulmonary function impairment.[3] Chronic pulmonary complications reported after treatment for pediatric malignancies include restrictive or obstructive chronic pulmonary disease, pulmonary fibrosis, and spontaneous pneumothorax.[6] These sequelae are uncommon after contemporary therapy, which most often results in subclinical injury that is detected only by imaging or formal pulmonary function testing. Pulmonary outcomes reported from selected cohort studies treated with thoracic radiation therapy include the following: - In a study of 48 survivors of pediatric malignant solid tumors with a median follow-up of 9.7 years after median whole-lung radiation doses of 12 Gy (range, 10.5-18 Gy), only nine patients (18.8%) reported respiratory symptoms. However, abnormalities in forced vital capacity, forced expiratory volume in 1 second, total lung capacity, and diffusion capacity were common (58%-73%). Focal-boost radiation therapy was also significantly associated with additional abnormalities.[7] Reducing the size of the daily radiation fractions (e.g., from 1.8 Gy per day to 1.5 Gy per day) decreases this risk.[8,9]
- For survivors of pediatric Hodgkin lymphoma, the prevalence of pulmonary symptoms using contemporary involved-field techniques is reported to be low. However, they still exhibit substantial subclinical dysfunction.[10]
- Changes in lung function have been reported in children treated with whole-lung radiation therapy for metastatic Wilms tumor. A dose of 12 Gy to 14 Gy reduced total lung capacity and vital capacity to about 70% of predicted values, and even lower if the patient had undergone thoracotomy.[8,9]
- Administration of bleomycin alone can produce pulmonary toxicity and, when combined with radiation therapy, can heighten radiation reactions. Chemotherapeutic agents such as doxorubicin, dactinomycin, and busulfan are radiomimetic agents and can reactivate latent radiation damage.[8,9,11]
Respiratory complications following chemotherapy Chemotherapy agents with potential pulmonary toxic effects commonly used in the treatment of pediatric malignancies include bleomycin, busulfan, and the nitrosoureas (carmustine and lomustine). These agents induce lung damage on their own or potentiate the damaging effects of radiation to the lung. Combined-modality therapy including pulmonary toxic chemotherapy and thoracic radiation therapy or thoracic/chest wall surgery increases the risk of pulmonary function impairment.[3] Outcomes observed among cohorts treated with pulmonary toxic chemotherapy include the following: - The development of bleomycin-associated pulmonary fibrosis with permanent restrictive disease is dose dependent, usually occurring at doses greater than 200 U/m2 to 400 U/m2, higher than those used in treatment protocols for pediatric malignancies.[11,12,13]
- More current pediatric regimens for Hodgkin lymphoma using radiation therapy and doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) have shown a significant incidence of asymptomatic pulmonary dysfunction after treatment, which appears to improve with time.[14,15,16] However, grades 3 and 4 pulmonary toxicity has been reported in 9% of children receiving 12 cycles of ABVD followed by 21 Gy of radiation.[13]
- ABVD-related pulmonary toxic effects may result from fibrosis induced by bleomycin or radiation recall pneumonitis related to administration of doxorubicin.
- Pulmonary veno-occlusive disease has been observed rarely and has been attributed to bleomycin chemotherapy.[17]
Respiratory complications associated with HSCT Patients undergoing HSCT are at increased risk of pulmonary toxic effects related to the following:[18,19,20] - Preexisting pulmonary dysfunction (e.g., asthma, pretransplant therapy).
- Conditioning regimens, including cyclophosphamide, busulfan, or carmustine.
- Total-body irradiation.
- Graft-versus-host disease (GVHD).
Although most survivors of transplant are not clinically compromised, restrictive lung disease may occur and has been reported to increase in prevalence with increasing time from HSCT, based on limited data from longitudinally followed cohorts.[21,22] Obstructive disease is less common, as is late onset pulmonary syndrome, which includes the spectrum of restrictive and obstructive disease. Bronchiolitis obliterans with or without organizing pneumonia, diffuse alveolar damage, and interstitial pneumonia may occur as a component of this syndrome, generally between 6 and 12 months posttransplant. Cough, dyspnea, or wheezing may occur with either normal chest x-ray or diffuse/patchy infiltrates; however, most patients are symptom free.[19,23,24] Other factors associated with respiratory late effects Additional factors contributing to chronic pulmonary toxic effects include superimposed infection, underlying pneumonopathy (e.g., asthma), respiratory toxic effects, chronic GVHD, and the effects of chronic pulmonary involvement by tumor or reaction to tumor. Lung lobectomy during childhood appears to have no significant impact on long-term pulmonary function,[25] but the long-term effect of lung surgery for children with cancer is not well defined. Pulmonary complications may also be exacerbated by smoking cigarettes or other substances. While smoking rates in survivors of childhood cancer tend to be lower than the general population, it is still important to prevent initiation of smoking and promote cessation in this distinct population.[26] Pulmonary function evaluations of 433 adult childhood cancer survivors treated with pulmonary toxic modalities demonstrated significantly higher risk for pulmonary dysfunction among smokers compared to nonsmokers. Forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) median values among current and former smokers were lower than those who had never smoked. Median FEV1/FVC values were lower among those who smoked less than 6 pack-years and those who smoked 6 pack-years or more compared with those who had never smoked suggesting that survivors who are former or current smokers have an increased risk for future obstructive and restrictive lung disease.[27] Table 15. Respiratory Late Effectsa| Predisposing Therapy | Respiratory Effects | Health Screening/Interventions |
|---|
| DLCO = diffusing capacity of the lung for carbon monoxide; GVHD = graft-versus-host disease. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Busulfan; carmustine (BCNU)/lomustine (CCNU); bleomycin; radiation impacting lungs; surgery impacting pulmonary function (lobectomy, metastasectomy, wedge resection) | Subclinical pulmonary dysfunction; interstitial pneumonitis; pulmonary fibrosis; restrictive lung disease; obstructive lung disease | History: cough, shortness of breath, dyspnea on exertion, wheezing | | Pulmonary exam | | Pulmonary function tests (including DLCO and spirometry) | | Chest x-ray | | Counsel regarding tobacco avoidance/smoking cessation | | In patients with abnormal pulmonary function tests and/or chest x-ray, consider repeat evaluation before general anesthesia | | Pulmonary consultation for patients with symptomatic pulmonary dysfunction | | Influenza and pneumococcal vaccinations | | Hematopoietic cell transplantation with any history of chronic GVHD | Pulmonary toxicity (bronchiolitis obliterans, chronic bronchitis, bronchiectasis) | History: cough, shortness of breath, dyspnea on exertion, wheezing | | Pulmonary exam | | Pulmonary function tests (including DLCO and spirometry) | | Chest x-ray | | Counsel regarding tobacco avoidance/smoking cessation | | In patients with abnormal pulmonary function tests and/or chest x-ray, consider repeat evaluation before general anesthesia | | Pulmonary consultation for patients with symptomatic pulmonary dysfunction | | Influenza and pneumococcal vaccinations | Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for respiratory late effects information including risk factors, evaluation, and health counseling.[28] References:
-
Mertens AC, Yasui Y, Liu Y, et al.: Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer 95 (11): 2431-41, 2002.
-
Huang TT, Chen Y, Dietz AC, et al.: Pulmonary outcomes in survivors of childhood central nervous system malignancies: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer 61 (2): 319-25, 2014.
-
Mulder RL, Thönissen NM, van der Pal HJ, et al.: Pulmonary function impairment measured by pulmonary function tests in long-term survivors of childhood cancer. Thorax 66 (12): 1065-71, 2011.
-
Armenian SH, Landier W, Francisco L, et al.: Long-term pulmonary function in survivors of childhood cancer. J Clin Oncol 33 (14): 1592-600, 2015.
-
Huang TT, Hudson MM, Stokes DC, et al.: Pulmonary outcomes in survivors of childhood cancer: a systematic review. Chest 140 (4): 881-901, 2011.
-
Josephson MB, Goldfarb SB: Pulmonary complications of childhood cancers. Expert Rev Respir Med 8 (5): 561-71, 2014.
-
Motosue MS, Zhu L, Srivastava K, et al.: Pulmonary function after whole lung irradiation in pediatric patients with solid malignancies. Cancer 118 (5): 1450-6, 2012.
-
McDonald S, Rubin P, Maasilta P: Response of normal lung to irradiation. Tolerance doses/tolerance volumes in pulmonary radiation syndromes. Front Radiat Ther Oncol 23: 255-76; discussion 299-301, 1989.
-
McDonald S, Rubin P, Phillips TL, et al.: Injury to the lung from cancer therapy: clinical syndromes, measurable endpoints, and potential scoring systems. Int J Radiat Oncol Biol Phys 31 (5): 1187-203, 1995.
-
Venkatramani R, Kamath S, Wong K, et al.: Pulmonary outcomes in patients with Hodgkin lymphoma treated with involved field radiation. Pediatr Blood Cancer 61 (7): 1277-81, 2014.
-
Kreisman H, Wolkove N: Pulmonary toxicity of antineoplastic therapy. Semin Oncol 19 (5): 508-20, 1992.
-
Bossi G, Cerveri I, Volpini E, et al.: Long-term pulmonary sequelae after treatment of childhood Hodgkin's disease. Ann Oncol 8 (Suppl 1): 19-24, 1997.
-
Fryer CJ, Hutchinson RJ, Krailo M, et al.: Efficacy and toxicity of 12 courses of ABVD chemotherapy followed by low-dose regional radiation in advanced Hodgkin's disease in children: a report from the Children's Cancer Study Group. J Clin Oncol 8 (12): 1971-80, 1990.
-
Hudson MM, Greenwald C, Thompson E, et al.: Efficacy and toxicity of multiagent chemotherapy and low-dose involved-field radiotherapy in children and adolescents with Hodgkin's disease. J Clin Oncol 11 (1): 100-8, 1993.
-
Hunger SP, Link MP, Donaldson SS: ABVD/MOPP and low-dose involved-field radiotherapy in pediatric Hodgkin's disease: the Stanford experience. J Clin Oncol 12 (10): 2160-6, 1994.
-
Marina NM, Greenwald CA, Fairclough DL, et al.: Serial pulmonary function studies in children treated for newly diagnosed Hodgkin's disease with mantle radiotherapy plus cycles of cyclophosphamide, vincristine, and procarbazine alternating with cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine. Cancer 75 (7): 1706-11, 1995.
-
Polliack A: Late therapy-induced cardiac and pulmonary complications in cured patients with Hodgkin's disease treated with conventional combination chemo-radiotherapy. Leuk Lymphoma 15 (Suppl 1): 7-10, 1995.
-
Cerveri I, Fulgoni P, Giorgiani G, et al.: Lung function abnormalities after bone marrow transplantation in children: has the trend recently changed? Chest 120 (6): 1900-6, 2001.
-
Leiper AD: Non-endocrine late complications of bone marrow transplantation in childhood: part II. Br J Haematol 118 (1): 23-43, 2002.
-
Marras TK, Chan CK, Lipton JH, et al.: Long-term pulmonary function abnormalities and survival after allogeneic marrow transplantation. Bone Marrow Transplant 33 (5): 509-17, 2004.
-
Inaba H, Yang J, Pan J, et al.: Pulmonary dysfunction in survivors of childhood hematologic malignancies after allogeneic hematopoietic stem cell transplantation. Cancer 116 (8): 2020-30, 2010.
-
Frisk P, Arvidson J, Hedenström H: A longitudinal study of pulmonary function after stem cell transplantation, from childhood to young adulthood. Pediatr Blood Cancer 58 (5): 775-9, 2012.
-
Uderzo C, Pillon M, Corti P, et al.: Impact of cumulative anthracycline dose, preparative regimen and chronic graft-versus-host disease on pulmonary and cardiac function in children 5 years after allogeneic hematopoietic stem cell transplantation: a prospective evaluation on behalf of the EBMT Pediatric Diseases and Late Effects Working Parties. Bone Marrow Transplant 39 (11): 667-75, 2007.
-
Yoshihara S, Yanik G, Cooke KR, et al.: Bronchiolitis obliterans syndrome (BOS), bronchiolitis obliterans organizing pneumonia (BOOP), and other late-onset noninfectious pulmonary complications following allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 13 (7): 749-59, 2007.
-
Kreisel D, Krupnick AS, Huddleston CB: Outcomes and late complications after pulmonary resections in the pediatric population. Semin Thorac Cardiovasc Surg 16 (3): 215-9, 2004.
-
Emmons K, Li FP, Whitton J, et al.: Predictors of smoking initiation and cessation among childhood cancer survivors: a report from the childhood cancer survivor study. J Clin Oncol 20 (6): 1608-16, 2002.
-
Oancea SC, Gurney JG, Ness KK, et al.: Cigarette smoking and pulmonary function in adult survivors of childhood cancer exposed to pulmonary-toxic therapy: results from the St. Jude lifetime cohort study. Cancer Epidemiol Biomarkers Prev 23 (9): 1938-43, 2014.
-
Liles A, Blatt J, Morris D, et al.: Monitoring pulmonary complications in long-term childhood cancer survivors: guidelines for the primary care physician. Cleve Clin J Med 75 (7): 531-9, 2008.
Late Effects of the Special SensesHearing Children treated for malignancies may be at risk for early- or delayed-onset hearing loss that can affect learning, communication, school performance, social interaction, and overall quality of life. In a study of adult survivors of pediatric central nervous system (CNS) tumors (n = 180) and non-CNS solid tumors (n = 226) who were treated with potentially ototoxic cancer therapy, serious hearing loss (requiring aid or resulting in deafness) was associated with a twofold increased risk of nonindependent living and unemployment or not graduating from high school.[1] The Children's Oncology Group has published recommendations for the evaluation and management of hearing loss in survivors of childhood and adolescent cancers to promote early identification of at-risk survivors and timely referral for remedial services.[2] Hearing loss as a late effect of therapy can occur after exposure to platinum compounds (cisplatin and carboplatin), cranial radiation therapy, or both. These therapeutic exposures are most common in the treatment of CNS and non-CNS solid tumors. Children are more susceptible to otologic toxic effects from platinum agents than are adults.[3,4] Risk factors associated with hearing loss include the following: - Younger age at treatment.
- Higher cumulative dose of platinum-based chemotherapy.
- Exposure to cisplatin combined with myeloablative carboplatin.[5]
- CNS tumors.
- Concomitant cranial radiation therapy.
Hearing loss and platinum-based therapy Platinum-related sensorineural hearing loss develops as an acute toxicity that is generally irreversible and bilateral. Hearing loss manifests initially in the high frequencies and progresses to the speech frequencies with increasing cumulative exposure. The prevalence of hearing loss has varied widely per series and is based on platinum treatment (e.g., platinum type, dose, infusion duration); host factors (e.g., age, genetic susceptibility, renal function); receipt of additional ototoxic therapy (cranial radiation therapy, aminoglycosides, loop diuretics), and the grading criteria used to report prevalence and severity of hearing loss.[6] - Cisplatin-induced hearing loss involving the speech frequencies (500-2000 Hz) usually occurs with cumulative doses that exceed 400 mg/m2 in pediatric patients.[5,7] Prolonging the duration of infusion or splitting the dose has been reported to reduce the risk of significant hearing loss.[8] Exposure to cisplatin combined with myeloablative carboplatin significantly increases the risk of severe hearing loss.[5] Otologic toxic effects after platinum chemotherapy have been reported to worsen years after completion of therapy.[9] Radiation therapy to the posterior fossa inclusive of the eighth cranial nerve (suggestive of damage to the cochlea at the end of therapy) increases the risk of late-onset hearing loss in survivors treated with cisplatin.[10]
- Carboplatin used in conventional (nonmyeloablative) dosing is typically not ototoxic.[11] However, delayed-onset hearing loss has been reported in specific populations. A single study of otologic toxic effects after non-stem cell transplant dosing of carboplatin for retinoblastoma reported that 8 of 175 children developed hearing loss. For seven of the eight children, the onset of the otologic toxic effects was delayed a median of 3.7 years.[12] Another study that evaluated audiological outcomes among 60 retinoblastoma survivors treated with nonmyeloablative systemic carboplatin and vincristine estimated a cumulative incidence of hearing loss of 20.3% at 10 years. Among the ten patients (17%) who developed sustained grade 3 or grade 4 hearing loss, nine were younger than 6 months at the start of chemotherapy. Younger age at the start of treatment was the only significant predictor of hearing loss; the cumulative incidence of hearing loss was 39% for patients younger than 6 months versus only 8.3% for patients aged 6 months and older.[13]
- The use of a carboplatin conditioning regimen for hematopoietic stem cell transplantation, particularly in combination with previous carboplatin or cisplatin therapy, may cause significant otologic toxic effects.[5,7]
Hearing loss and cranial radiation therapy Cranial radiation therapy, when used as a single modality, may result in otologic toxic effects that may be gradual in onset, manifesting months to years after exposure. The threshold dose for auditory toxicity after radiation therapy alone is in the range of 35 to 45 Gy for children.[14] High-frequency sensorineural hearing loss is uncommon at cumulative radiation doses below 35 Gy, and is rarely severe below doses of 45 Gy.[15] The exception is for patients with supratentorial tumors and ventriculoperitoneal shunts, in whom doses below 30 Gy may be associated with intermediate frequency (1,000-2,000 Hz) hearing loss.[14,16] To reduce the risk of hearing loss, the average cochlear dose should not exceed 30 to 35 Gy, delivered over 6 weeks. Young patient age and presence of a brain tumor and/or hydrocephalus can increase susceptibility to hearing loss. Sensorineural hearing loss after cranial radiation therapy can progress over time. In a study of 235 pediatric brain tumor patients treated with conformal or intensity-modulated radiation therapy (without cisplatin or pre-existing hearing loss) and monitored for a median of 9 years, sensorineural hearing loss was prevalent in 14% of patients, with a median time to onset of 3.6 years from radiation therapy. Follow-up evaluations among 29 patients identified continued decline in hearing sensitivity. Risk factors for cranial radiation-associated sensorineural hearing loss included younger age at initiation of radiation, higher cochlear radiation dose, and cerebrospinal fluid shunting.[17] When used concomitantly with cisplatin, radiation therapy can substantially exacerbate the hearing loss associated with platinum chemotherapy.[14,18,19,20] In a report from the Childhood Cancer Survivor Study (CCSS), 5-year survivors were at increased risk of problems with hearing sounds (relative risk [RR], 2.3), tinnitus (RR, 1.7), hearing loss requiring an aid (RR, 4.4), and hearing loss in one or both ears not corrected by a hearing aid (RR, 5.2), compared with siblings. Temporal lobe irradiation (>30 Gy) and posterior fossa irradiation (>50 Gy but also 30-49.9 Gy) were associated with these adverse outcomes. Exposure to platinum was associated with an increased risk of problems with hearing sounds (RR, 2.1), tinnitus (RR, 2.8), and hearing loss requiring an aid (RR, 4.1).[21] Table 16. Auditory Late Effectsa| Predisposing Therapy | Potential Auditory Effects | Health Screening/Interventions |
|---|
| FM = frequency modulated. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Platinum agents (cisplatin, carboplatin); radiation impacting the ear | Otologic toxic effects; sensorineural hearing loss; tinnitus; vertigo; dehydrated ceruminosis; conductive hearing loss | History: hearing difficulties, tinnitus, vertigo | | Otoscopic exam | | Audiology evaluation | | Amplification in patients with progressive hearing loss | | Speech and language therapy for children with hearing loss | | Otolaryngology consultation in patients with chronic infection, cerumen impaction, or other anatomical problems exacerbating or contributing to hearing loss | | Educational accommodations (e.g., preferential classroom seating, FM amplification system, etc.) | Orbital and Optic Orbital complications are common after radiation therapy for retinoblastoma and after total-body irradiation (TBI) and in children with head and neck sarcomas and CNS tumors. Retinoblastoma For survivors of retinoblastoma, a small orbital volume may result from either enucleation or radiation therapy. Age younger than 1 year may increase risk, but this finding is not consistent across studies.[22,23] Progress has been made in the management of retinoblastoma, with better enucleation implants, intravenous chemoreduction, and intra-arterial chemotherapy in addition to thermotherapy, cryotherapy, and plaque radiation therapy. Longer follow-up is needed to assess the impact on vision in patients undergoing these more contemporary treatment modalities.[22,24,25] Previously, tumors located near the macula and fovea were associated with an increased risk of complications leading to vision loss, although treatment of these tumors with foveal laser ablation has shown promise in preserving vision.[26,27,28,29] (Refer to the PDQ summary on Retinoblastoma Treatment for more information on the treatment of retinoblastoma.) Rhabdomyosarcoma Survivors of orbital rhabdomyosarcoma are at risk of dry eye, cataract, orbital hypoplasia, ptosis, retinopathy, keratoconjunctivitis, optic neuropathy, lid epithelioma, and impairment of vision after radiation therapy doses of 30 Gy to 65 Gy. The higher dose ranges (>50 Gy) are associated with lid epitheliomas, keratoconjunctivitis, lacrimal duct atrophy, and severe dry eye. Retinitis and optic neuropathy may also result from doses of 50 Gy to 65 Gy and even at lower total doses if the individual fraction size is higher than 2 Gy.[30] Cataracts are reported after lower doses of 10 Gy to 18 Gy.[31,32,33] (Refer to the PDQ summary on Childhood Rhabdomyosarcoma Treatment for more information on the treatment of rhabdomyosarcoma in children.) Low-grade optic pathway glioma and craniopharyngioma Survivors of optic pathway glioma and craniopharyngioma are also at risk of visual complications, resulting in part from tumor proximity to the optic nerve. Longitudinal follow-up (mean, 9 years) of 21 patients with optic pathway gliomas indicated that before treatment, 81% of patients had reduced visual acuity, 81% had optic nerve pallor, and all had reduced visual evoked potentials in one or both eyes. Treatment arrested acuity loss for 4 to 5 years. Visual acuity was stable or improved in 33% of patients at last follow-up; however, it declined on average. Visual acuity at follow-up was related to tumor volume at initial presentation.[34] In a study of 25 patients diagnosed with craniopharyngioma, 67% had visual complications at a mean follow-up of 11 years.[35] A retrospective review of 30 children with craniopharyngioma revealed that 19 patients had vision loss before surgery; 21 patients had postsurgical vision loss. Preoperative vision loss was predicative of postoperative vision loss.[36] CCSS investigators evaluated the impact of impaired vision on cognitive and psychosocial outcomes among 1,233 adult survivors of childhood low-grade gliomas. Some degree of visual impairment was prevalent in 22.5% of patients, and 3.8% of patients were blind in both eyes. Survivors who were blind in both eyes were more likely to be unmarried, live dependently, and be unemployed than were those with unimpaired vision. However, bilateral blindness did not impact cognitive or emotional outcomes. Impaired (with some remaining) vision was not associated with psychological or economic outcomes.[37] Treatment-specific effects Survivors of childhood cancer are at increased risk for ocular late effects related to both glucocorticoid and radiation exposure to the eye. The CCSS reported that survivors who were 5 or more years from diagnosis were at increased risk for cataracts (RR, 10.8), glaucoma (RR, 2.5), legal blindness (RR, 2.6), double vision (RR, 4.1), and dry eye (RR, 1.9), compared with siblings. The dose of radiation to the eye is significantly associated with risk of cataracts, legal blindness, double vision, and dry eye, in a dose-dependent manner. Risk of cataracts was associated with a radiation dose of 30 Gy or more to the posterior fossa and temporal lobe and treatment with prednisone. The cumulative incidence of cataracts, double vision, dry eye, and legal blindness continued to increase up to 20 years after diagnosis for those who received more than 5 Gy to the eye.[38] The 15-year cumulative incidence of cataract was 4.5% among 517 survivors of childhood acute lymphoblastic leukemia (median, 10.9 years from diagnosis), systematically evaluated by slit lamp examination. CNS radiation therapy was the only treatment-related risk factor identified for cataract development, which occurred in 11.1% of irradiated survivors, compared with 2.8% of those who were not irradiated.[39] Ocular complications, such as cataracts and dry-eye syndrome, are common after stem cell transplantation in childhood. Compared with patients treated with busulfan or other chemotherapy, patients treated with single-dose or fractionated TBI are at increased risk of cataracts. Risk ranges from approximately 10% to 60% at 10 years posttreatment, depending on the total dose and fractionation, with a shorter latency period and more severe cataracts noted after single fraction and higher dose or dose-rate TBI.[40,41,42,43] Patients receiving TBI doses of less than 40 Gy have a less than 10% chance of developing severe cataracts.[43] Corticosteroids and graft-versus-host disease may further increase risk.[40,44] The prevalence of cataracts, evaluated by serial slit lamp testing, among 271 participants (mean follow-up, 10.3 years) in the Leucémie Enfants Adolescents (LEA) program was 41.7%, with 8.1% requiring surgical intervention.[45] In this cohort, the cumulative incidence of cataracts among those treated with TBI increased over time from 30% at 5 years to 70.8% at 15 years and 78% at 20 years. The lack of a plateau in cataract incidence suggests that nearly all patients treated with TBI will develop cataracts as follow-up increases. In contrast, the 15-year cumulative incidence of cataracts was 12.5% among those conditioned with busulfan. Multivariable analysis identified high cumulative steroid dose as a potential cofactor with TBI for cataract risk. Epithelial superficial keratopathy has been shown to be more common if the patient was exposed to repeated high trough levels of cyclosporine A.[46] Table 17. Ocular Late Effectsa| Predisposing Therapy | Ocular/Vision Effects | Health Screening/Interventions |
|---|
| GVHD = graft-versus-host disease. | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Busulfan; corticosteroids; radiation impacting the eye | Cataracts | History: decreased acuity, halos, diplopia | | Eye exam: visual acuity, funduscopy | | Ophthalmology consultation | | Radiation impacting the eye, including radioiodine (I-131) | Ocular toxicity (orbital hypoplasia, lacrimal duct atrophy, xerophthalmia [keratoconjunctivitis sicca], keratitis, telangiectasias, retinopathy, optic chiasm neuropathy, enophthalmos, chronic painful eye, maculopathy, papillopathy, glaucoma) | History: visual changes (decreased acuity, halos, diplopia), dry eye, persistent eye irritation, excessive tearing, light sensitivity, poor night vision, painful eye | | Eye exam: visual acuity, funduscopy | | Ophthalmology consultation | | Hematopoietic cell transplantation with any history of chronic GVHD | Xerophthalmia (keratoconjunctivitis sicca) | History: dry eye (burning, itching, foreign body sensation, inflammation) | | Eye exam: visual acuity, funduscopy | | Enucleation | Impaired cosmesis; poor prosthetic fit; orbital hypoplasia | Ocular prosthetic evaluation | | Ophthalmology | Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for information on the late effects of special senses, including risk factors, evaluation, and health counseling. References:
-
Brinkman TM, Bass JK, Li Z, et al.: Treatment-induced hearing loss and adult social outcomes in survivors of childhood CNS and non-CNS solid tumors: Results from the St. Jude Lifetime Cohort Study. Cancer 121 (22): 4053-61, 2015.
-
Bass JK, Knight KR, Yock TI, et al.: Evaluation and Management of Hearing Loss in Survivors of Childhood and Adolescent Cancers: A Report From the Children's Oncology Group. Pediatr Blood Cancer 63 (7): 1152-62, 2016.
-
Grewal S, Merchant T, Reymond R, et al.: Auditory late effects of childhood cancer therapy: a report from the Children's Oncology Group. Pediatrics 125 (4): e938-50, 2010.
-
Li Y, Womer RB, Silber JH: Predicting cisplatin ototoxicity in children: the influence of age and the cumulative dose. Eur J Cancer 40 (16): 2445-51, 2004.
-
Landier W, Knight K, Wong FL, et al.: Ototoxicity in children with high-risk neuroblastoma: prevalence, risk factors, and concordance of grading scales--a report from the Children's Oncology Group. J Clin Oncol 32 (6): 527-34, 2014.
-
Brock PR, Knight KR, Freyer DR, et al.: Platinum-induced ototoxicity in children: a consensus review on mechanisms, predisposition, and protection, including a new International Society of Pediatric Oncology Boston ototoxicity scale. J Clin Oncol 30 (19): 2408-17, 2012.
-
Kushner BH, Budnick A, Kramer K, et al.: Ototoxicity from high-dose use of platinum compounds in patients with neuroblastoma. Cancer 107 (2): 417-22, 2006.
-
Lewis MJ, DuBois SG, Fligor B, et al.: Ototoxicity in children treated for osteosarcoma. Pediatr Blood Cancer 52 (3): 387-91, 2009.
-
Bertolini P, Lassalle M, Mercier G, et al.: Platinum compound-related ototoxicity in children: long-term follow-up reveals continuous worsening of hearing loss. J Pediatr Hematol Oncol 26 (10): 649-55, 2004.
-
Kolinsky DC, Hayashi SS, Karzon R, et al.: Late onset hearing loss: a significant complication of cancer survivors treated with Cisplatin containing chemotherapy regimens. J Pediatr Hematol Oncol 32 (2): 119-23, 2010.
-
Fouladi M, Gururangan S, Moghrabi A, et al.: Carboplatin-based primary chemotherapy for infants and young children with CNS tumors. Cancer 115 (14): 3243-53, 2009.
-
Jehanne M, Lumbroso-Le Rouic L, Savignoni A, et al.: Analysis of ototoxicity in young children receiving carboplatin in the context of conservative management of unilateral or bilateral retinoblastoma. Pediatr Blood Cancer 52 (5): 637-43, 2009.
-
Qaddoumi I, Bass JK, Wu J, et al.: Carboplatin-associated ototoxicity in children with retinoblastoma. J Clin Oncol 30 (10): 1034-41, 2012.
-
Hua C, Bass JK, Khan R, et al.: Hearing loss after radiotherapy for pediatric brain tumors: effect of cochlear dose. Int J Radiat Oncol Biol Phys 72 (3): 892-9, 2008.
-
Bhandare N, Jackson A, Eisbruch A, et al.: Radiation therapy and hearing loss. Int J Radiat Oncol Biol Phys 76 (3 Suppl): S50-7, 2010.
-
Merchant TE, Gould CJ, Xiong X, et al.: Early neuro-otologic effects of three-dimensional irradiation in children with primary brain tumors. [Abstract] Int J Radiat Oncol Biol Phys 54 (Suppl 2): A-1073, 201, 2002.
-
Bass JK, Hua CH, Huang J, et al.: Hearing Loss in Patients Who Received Cranial Radiation Therapy for Childhood Cancer. J Clin Oncol 34 (11): 1248-55, 2016.
-
Cheuk DK, Billups CA, Martin MG, et al.: Prognostic factors and long-term outcomes of childhood nasopharyngeal carcinoma. Cancer 117 (1): 197-206, 2011.
-
Merchant TE, Hua CH, Shukla H, et al.: Proton versus photon radiotherapy for common pediatric brain tumors: comparison of models of dose characteristics and their relationship to cognitive function. Pediatr Blood Cancer 51 (1): 110-7, 2008.
-
Paulino AC, Lobo M, Teh BS, et al.: Ototoxicity after intensity-modulated radiation therapy and cisplatin-based chemotherapy in children with medulloblastoma. Int J Radiat Oncol Biol Phys 78 (5): 1445-50, 2010.
-
Whelan K, Stratton K, Kawashima T, et al.: Auditory complications in childhood cancer survivors: a report from the childhood cancer survivor study. Pediatr Blood Cancer 57 (1): 126-34, 2011.
-
Kaste SC, Chen G, Fontanesi J, et al.: Orbital development in long-term survivors of retinoblastoma. J Clin Oncol 15 (3): 1183-9, 1997.
-
Peylan-Ramu N, Bin-Nun A, Skleir-Levy M, et al.: Orbital growth retardation in retinoblastoma survivors: work in progress. Med Pediatr Oncol 37 (5): 465-70, 2001.
-
Shields CL, Shields JA: Retinoblastoma management: advances in enucleation, intravenous chemoreduction, and intra-arterial chemotherapy. Curr Opin Ophthalmol 21 (3): 203-12, 2010.
-
Abramson DH, Dunkel IJ, Brodie SE, et al.: Superselective ophthalmic artery chemotherapy as primary treatment for retinoblastoma (chemosurgery). Ophthalmology 117 (8): 1623-9, 2010.
-
Shields CL, Shields JA: Recent developments in the management of retinoblastoma. J Pediatr Ophthalmol Strabismus 36 (1): 8-18; quiz 35-6, 1999 Jan-Feb.
-
Shields CL, Shields JA, Cater J, et al.: Plaque radiotherapy for retinoblastoma: long-term tumor control and treatment complications in 208 tumors. Ophthalmology 108 (11): 2116-21, 2001.
-
Shields JA, Shields CL: Pediatric ocular and periocular tumors. Pediatr Ann 30 (8): 491-501, 2001.
-
Schefler AC, Cicciarelli N, Feuer W, et al.: Macular retinoblastoma: evaluation of tumor control, local complications, and visual outcomes for eyes treated with chemotherapy and repetitive foveal laser ablation. Ophthalmology 114 (1): 162-9, 2007.
-
Kline LB, Kim JY, Ceballos R: Radiation optic neuropathy. Ophthalmology 92 (8): 1118-26, 1985.
-
Paulino AC, Simon JH, Zhen W, et al.: Long-term effects in children treated with radiotherapy for head and neck rhabdomyosarcoma. Int J Radiat Oncol Biol Phys 48 (5): 1489-95, 2000.
-
Oberlin O, Rey A, Anderson J, et al.: Treatment of orbital rhabdomyosarcoma: survival and late effects of treatment--results of an international workshop. J Clin Oncol 19 (1): 197-204, 2001.
-
Raney RB, Anderson JR, Kollath J, et al.: Late effects of therapy in 94 patients with localized rhabdomyosarcoma of the orbit: Report from the Intergroup Rhabdomyosarcoma Study (IRS)-III, 1984-1991. Med Pediatr Oncol 34 (6): 413-20, 2000.
-
Kelly JP, Leary S, Khanna P, et al.: Longitudinal measures of visual function, tumor volume, and prediction of visual outcomes after treatment of optic pathway gliomas. Ophthalmology 119 (6): 1231-7, 2012.
-
Poretti A, Grotzer MA, Ribi K, et al.: Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol 46 (4): 220-9, 2004.
-
Fisher PG, Jenab J, Gopldthwaite PT, et al.: Outcomes and failure patterns in childhood craniopharyngiomas. Childs Nerv Syst 14 (10): 558-63, 1998.
-
de Blank PM, Fisher MJ, Lu L, et al.: Impact of vision loss among survivors of childhood central nervous system astroglial tumors. Cancer 122 (5): 730-9, 2016.
-
Whelan KF, Stratton K, Kawashima T, et al.: Ocular late effects in childhood and adolescent cancer survivors: a report from the childhood cancer survivor study. Pediatr Blood Cancer 54 (1): 103-9, 2010.
-
Alloin AL, Barlogis V, Auquier P, et al.: Prevalence and risk factors of cataract after chemotherapy with or without central nervous system irradiation for childhood acute lymphoblastic leukaemia: an LEA study. Br J Haematol 164 (1): 94-100, 2014.
-
Ferry C, Gemayel G, Rocha V, et al.: Long-term outcomes after allogeneic stem cell transplantation for children with hematological malignancies. Bone Marrow Transplant 40 (3): 219-24, 2007.
-
Fahnehjelm KT, Törnquist AL, Olsson M, et al.: Visual outcome and cataract development after allogeneic stem-cell transplantation in children. Acta Ophthalmol Scand 85 (7): 724-33, 2007.
-
Gurney JG, Ness KK, Rosenthal J, et al.: Visual, auditory, sensory, and motor impairments in long-term survivors of hematopoietic stem cell transplantation performed in childhood: results from the Bone Marrow Transplant Survivor study. Cancer 106 (6): 1402-8, 2006.
-
Kal HB, VAN Kempen-Harteveld ML: Induction of severe cataract and late renal dysfunction following total body irradiation: dose-effect relationships. Anticancer Res 29 (8): 3305-9, 2009.
-
Holmström G, Borgström B, Calissendorff B: Cataract in children after bone marrow transplantation: relation to conditioning regimen. Acta Ophthalmol Scand 80 (2): 211-5, 2002.
-
Horwitz M, Auquier P, Barlogis V, et al.: Incidence and risk factors for cataract after haematopoietic stem cell transplantation for childhood leukaemia: an LEA study. Br J Haematol 168 (4): 518-25, 2015.
-
Fahnehjelm KT, Törnquist AL, Winiarski J: Dry-eye syndrome after allogeneic stem-cell transplantation in children. Acta Ophthalmol 86 (3): 253-8, 2008.
Late Effects of the Urinary SystemAcute toxicity of the urinary system from cancer therapy is well known. Less is known about the genitourinary outcomes in long-term survivors.[1] The evidence for long-term renal injury in childhood cancer survivors is limited by studies characterized by small sample size, cohort selection and participation bias, cross-sectional assessment, heterogeneity in time since treatment, and method of ascertainment. In particular, the inaccuracies of diagnosing chronic kidney dysfunction by estimating equations of glomerular dysfunction should be considered.[2] Cancer treatments predisposing to renal injury and/or high blood pressure later in life include chemotherapeutic drugs (cisplatin, carboplatin, ifosfamide, methotrexate), renal radiation therapy, and nephrectomy. The risk and the degree of renal dysfunction depend on type and intensity of therapy and interpretation of the studies is compromised by variability in testing. Few large-scale studies have evaluated late renal-health outcomes and risk factors for renal dysfunction among survivors treated with potentially nephrotoxic modalities. In a large cross-sectional study of 1,442 childhood cancer survivors (median attained age, 19.3 years; median time from diagnosis, 12.1 years), Dutch investigators assessed the presence of albuminuria, hypomagnesemia, hypophosphatemia, and hypertension and estimated glomerular filtration rate (GFR) among survivors treated with ifosfamide, cisplatin, carboplatin, high-dose cyclophosphamide (>1 g/m2 or more per course), or high-dose methotrexate (>1 g/m2 or more per course), radiation therapy to the kidney region, total-body irradiation (TBI), or nephrectomy. At least one abnormality of renal function or hypertension was detected in 28.1% of survivors. History of nephrectomy (odds ratio [OR], 8.6; 95% confidence interval [CI], 3.4-21.4) had the strongest association with a GFR of less than 90 ml/min per 1.73 m2. The prevalence of decreased GFR was highest among those treated with multimodality therapy including nephrectomy, nephrotoxic chemotherapy, and abdominal radiation therapy. Nearly 5% of these survivors had a GFR of less than 90 ml/min per 1.73 m2. Abdominal irradiation was the only significant treatment-related risk factor for hypertension (OR, 2.5; 95% CI, 1.4-4.5).[3] Therapy-related factors affecting the kidney Cancer treatments predisposing to late renal injury and hypertension include the following:[4,5,6] Genetic factors predisposing to renal dysfunction Many childhood survivors of Wilms tumor who develop chronic renal failure have syndromes accompanying WT1 mutations or deletions that predispose to renal disease. Data from the National Wilms Tumor Study Group and the U.S. Renal Data System indicate that the 20-year cumulative incidence of end-stage renal disease in children with unilateral Wilms tumor and Denys-Drash syndrome is 74%, 36% for those with WAGR (Wilms tumor, aniridia, genitourinary abnormalities, mental retardation) syndrome, 7% for male patients with genitourinary anomalies, and 0.6% for 5,347 patients with none of these conditions.[28] For patients with bilateral Wilms tumors, the incidence of end-stage renal disease is 50% for Denys-Drash syndrome, 90% for WAGR, 25% for genitourinary anomaly, and 12% for patients for all others.[28,29] End-stage renal disease in patients with WAGR and genitourinary anomalies tended to occur relatively late, and often during or after adolescence.[28] Therapy-related bladder complications Pelvic or central nervous system surgery, alkylator-containing chemotherapy including cyclophosphamide or ifosfamide, pelvic radiation therapy, and certain spinal and genitourinary surgical procedures have been associated with the following urinary bladder late effects:[30] - Chemotherapy. The oxazophorine alkylating agents (cyclophosphamide and ifosfamide) and radiation therapy exposing the bladder have been implicated in the development of hemorrhagic cystitis. Chemotherapy-associated hemorrhagic cystitis presents as an acute toxicity and appears to be a rare persistent effect among clinically well characterized long-term survivor cohorts.[31,32] In a study of 6,119 children treated between 1986 and 2010 (mean age, 12.2 years ± 6.3 SD), 1.6% (n = 97) developed hemorrhagic cystitis, most of whom (75%) had severity scores of II or III (scale, I-IV). Patients with radiological evidence of renal or bladder calculi or tumors invading the bladder wall were excluded from the study. Older age, previous bone marrow or peripheral stem cell transplantation, and BK virus in the urine were risk factors for hemorrhagic cystitis and were associated with a higher severity score.[33]
Previous exposure to cyclophosphamide has been linked to risk of bladder carcinoma. An excess prevalence of bladder tumors has also been observed in survivors of specific diagnostic types (e.g., heritable retinoblastoma) supporting the contribution of genetic factors in the development of subsequent neoplasms.[34,35] - Radiation therapy. Pelvic radiation therapy is also associated with an increased risk of hemorrhagic cystitis that may be either acute or chronic in presentation. The risk of radiation-induced hemorrhagic cystitis is greatest among survivors treated with radiation doses of more than 30 Gy to the whole bladder or more than 60 Gy to a portion of the bladder. Long-term bladder fibrosis and contracture may result as a sequelae of hemorrhagic cystitis or radiation therapy.[30]
- Surgery. Surgical procedures involving the lower genitourinary tract have the potential to impair normal function of the bladder and normal voiding mechanisms. Likewise, any cancer therapy or tumor infiltration that disrupts innervation of the bladder can have deleterious effects on bladder function that may manifest as impaired bladder storage, inability to void and/or incontinence.
Table 18. Kidney and Bladder Late Effectsa| Predisposing Therapy | Renal/Genitourinary Effects | Health Screening |
|---|
| BUN = blood urea nitrogen; NSAIDs = nonsteroidal anti-inflammatory drugs; RBC/HFP = red blood cells per high-field power (microscopic exam). | | a Adapted from theChildren's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. | | Cisplatin/carboplatin; ifosfamide | Renal toxicity (glomerular injury, tubular injury [renal tubular acidosis], Fanconi syndrome, hypophosphatemic rickets) | Blood pressure | | BUN, Creatinine, Na, K, Cl, CO2, Ca, Mg, PO4 levels | | Urinalysis | | Electrolyte supplements for patients with persistent electrolyte wasting | | Nephrology consultation for patients with hypertension, proteinuria, or progressive renal insufficiency | | Methotrexate; radiation impacting kidneys/urinary tract | Renal toxicity (renal insufficiency, hypertension) | Blood pressure | | BUN, Creatinine, Na, K, Cl, CO2, Ca, Mg, PO4 levels | | Urinalysis | | Nephrology consultation for patients with hypertension, proteinuria, or progressive renal insufficiency | | Nephrectomy | Renal toxicity (proteinuria, hyperfiltration, renal insufficiency) | Blood pressure | | BUN, Creatinine, Na, K, Cl, CO2, Ca, Mg, PO4 levels | | Urinalysis | | Discuss contact sports, bicycle safety (e.g., avoiding handlebar injuries), and proper use of seatbelts (i.e., wearing lap belts around hips, not waist) | | Counsel to use NSAIDs with caution | | Nephrology consultation for patients with hypertension, proteinuria, or progressive renal insufficiency | | Nephrectomy; pelvic surgery; cystectomy | Hydrocele | Testicular exam | | Cystectomy | Cystectomy-related complications (chronic urinary tract infections, renal dysfunction, vesicoureteral reflux, hydronephrosis, reservoir calculi, spontaneous neobladder perforation, vitamin B12 /folate/carotene deficiency [patients with ileal enterocystoplasty only]) | Urology evaluation | | Vitamin B12 level | | Pelvic surgery; cystectomy | Urinary incontinence; urinary tract obstruction | History: hematuria, urinary urgency/frequency, urinary incontinence/retention, dysuria, nocturia, abnormal urinary stream | | Counsel regarding adequate fluid intake, regular voiding, seeking medical attention for symptoms of voiding dysfunction or urinary tract infection, compliance with recommended bladder catheterization regimen | | Urologic consultation for patients with dysfunctional voiding or recurrent urinary tract infections | | Cyclophosphamide/Ifosfamide; radiation impacting bladder/urinary tract | Bladder toxicity (hemorrhagic cystitis, bladder fibrosis, dysfunctional voiding, vesicoureteral reflux, hydronephrosis) | History: hematuria, urinary urgency/frequency, urinary incontinence/retention, dysuria, nocturia, abnormal urinary stream | | Urinalysis | | Urine culture, spot urine calcium/creatinine ratio, and ultrasound of kidneys and bladder for patients with microscopic hematuria (defined as ≥5 RBC/HFP on at least 2 occasions) | | Nephrology or urology referral for patients with culture-negative microscopic hematuria AND abnormal ultrasound and/or abnormal calcium/creatinine ratio | | Urology referral for patients with culture negative macroscopic hematuria | Refer to the Children's Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers for urinary late effects information including risk factors, evaluation, and health counseling. References:
-
Shnorhavorian M, Friedman DL, Koyle MA: Genitourinary long-term outcomes for childhood cancer survivors. Curr Urol Rep 10 (2): 134-7, 2009.
-
Green DM: Evaluation of renal function after successful treatment for unilateral, non-syndromic Wilms tumor. Pediatr Blood Cancer 60 (12): 1929-35, 2013.
-
Knijnenburg SL, Jaspers MW, van der Pal HJ, et al.: Renal dysfunction and elevated blood pressure in long-term childhood cancer survivors. Clin J Am Soc Nephrol 7 (9): 1416-27, 2012.
-
Jones DP, Spunt SL, Green D, et al.: Renal late effects in patients treated for cancer in childhood: a report from the Children's Oncology Group. Pediatr Blood Cancer 51 (6): 724-31, 2008.
-
Dekkers IA, Blijdorp K, Cransberg K, et al.: Long-term nephrotoxicity in adult survivors of childhood cancer. Clin J Am Soc Nephrol 8 (6): 922-9, 2013.
-
Mulder RL, Knijnenburg SL, Geskus RB, et al.: Glomerular function time trends in long-term survivors of childhood cancer: a longitudinal study. Cancer Epidemiol Biomarkers Prev 22 (10): 1736-46, 2013.
-
Interiano RB, Delos Santos N, Huang S, et al.: Renal function in survivors of nonsyndromic Wilms tumor treated with unilateral radical nephrectomy. Cancer 121 (14): 2449-56, 2015.
-
Marina NM, Poquette CA, Cain AM, et al.: Comparative renal tubular toxicity of chemotherapy regimens including ifosfamide in patients with newly diagnosed sarcomas. J Pediatr Hematol Oncol 22 (2): 112-8, 2000 Mar-Apr.
-
Hartmann JT, Fels LM, Franzke A, et al.: Comparative study of the acute nephrotoxicity from standard dose cisplatin +/- ifosfamide and high-dose chemotherapy with carboplatin and ifosfamide. Anticancer Res 20 (5C): 3767-73, 2000 Sep-Oct.
-
Skinner R, Parry A, Price L, et al.: Persistent nephrotoxicity during 10-year follow-up after cisplatin or carboplatin treatment in childhood: relevance of age and dose as risk factors. Eur J Cancer 45 (18): 3213-9, 2009.
-
Skinner R, Kaplan R, Nathan PC: Renal and pulmonary late effects of cancer therapy. Semin Oncol 40 (6): 757-73, 2013.
-
Stöhr W, Paulides M, Bielack S, et al.: Nephrotoxicity of cisplatin and carboplatin in sarcoma patients: a report from the late effects surveillance system. Pediatr Blood Cancer 48 (2): 140-7, 2007.
-
Skinner R, Cotterill SJ, Stevens MC: Risk factors for nephrotoxicity after ifosfamide treatment in children: a UKCCSG Late Effects Group study. United Kingdom Children's Cancer Study Group. Br J Cancer 82 (10): 1636-45, 2000.
-
Stöhr W, Paulides M, Bielack S, et al.: Ifosfamide-induced nephrotoxicity in 593 sarcoma patients: a report from the Late Effects Surveillance System. Pediatr Blood Cancer 48 (4): 447-52, 2007.
-
Oberlin O, Fawaz O, Rey A, et al.: Long-term evaluation of Ifosfamide-related nephrotoxicity in children. J Clin Oncol 27 (32): 5350-5, 2009.
-
Widemann BC, Balis FM, Kim A, et al.: Glucarpidase, leucovorin, and thymidine for high-dose methotrexate-induced renal dysfunction: clinical and pharmacologic factors affecting outcome. J Clin Oncol 28 (25): 3979-86, 2010.
-
Cohen EP, Robbins ME: Radiation nephropathy. Semin Nephrol 23 (5): 486-99, 2003.
-
Dawson LA, Kavanagh BD, Paulino AC, et al.: Radiation-associated kidney injury. Int J Radiat Oncol Biol Phys 76 (3 Suppl): S108-15, 2010.
-
Mitus A, Tefft M, Fellers FX: Long-term follow-up of renal functions of 108 children who underwent nephrectomy for malignant disease. Pediatrics 44 (6): 912-21, 1969.
-
Bölling T, Ernst I, Pape H, et al.: Dose-volume analysis of radiation nephropathy in children: preliminary report of the risk consortium. Int J Radiat Oncol Biol Phys 80 (3): 840-4, 2011.
-
Peschel RE, Chen M, Seashore J: The treatment of massive hepatomegaly in stage IV-S neuroblastoma. Int J Radiat Oncol Biol Phys 7 (4): 549-53, 1981.
-
Ritchey ML, Green DM, Thomas PR, et al.: Renal failure in Wilms' tumor patients: a report from the National Wilms' Tumor Study Group. Med Pediatr Oncol 26 (2): 75-80, 1996.
-
Paulino AC, Wilimas J, Marina N, et al.: Local control in synchronous bilateral Wilms tumor. Int J Radiat Oncol Biol Phys 36 (3): 541-8, 1996.
-
Cheng JC, Schultheiss TE, Wong JY: Impact of drug therapy, radiation dose, and dose rate on renal toxicity following bone marrow transplantation. Int J Radiat Oncol Biol Phys 71 (5): 1436-43, 2008.
-
Hoffmeister PA, Hingorani SR, Storer BE, et al.: Hypertension in long-term survivors of pediatric hematopoietic cell transplantation. Biol Blood Marrow Transplant 16 (4): 515-24, 2010.
-
Abboud I, Porcher R, Robin M, et al.: Chronic kidney dysfunction in patients alive without relapse 2 years after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 15 (10): 1251-7, 2009.
-
Ellis MJ, Parikh CR, Inrig JK, et al.: Chronic kidney disease after hematopoietic cell transplantation: a systematic review. Am J Transplant 8 (11): 2378-90, 2008.
-
Breslow NE, Collins AJ, Ritchey ML, et al.: End stage renal disease in patients with Wilms tumor: results from the National Wilms Tumor Study Group and the United States Renal Data System. J Urol 174 (5): 1972-5, 2005.
-
Hamilton TE, Ritchey ML, Haase GM, et al.: The management of synchronous bilateral Wilms tumor: a report from the National Wilms Tumor Study Group. Ann Surg 253 (5): 1004-10, 2011.
-
Ritchey M, Ferrer F, Shearer P, et al.: Late effects on the urinary bladder in patients treated for cancer in childhood: a report from the Children's Oncology Group. Pediatr Blood Cancer 52 (4): 439-46, 2009.
-
Hudson MM, Ness KK, Gurney JG, et al.: Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 309 (22): 2371-81, 2013.
-
Landier W, Armenian SH, Lee J, et al.: Yield of screening for long-term complications using the children's oncology group long-term follow-up guidelines. J Clin Oncol 30 (35): 4401-8, 2012.
-
Riachy E, Krauel L, Rich BS, et al.: Risk factors and predictors of severity score and complications of pediatric hemorrhagic cystitis. J Urol 191 (1): 186-92, 2014.
-
Kersun LS, Wimmer RS, Hoot AC, et al.: Secondary malignant neoplasms of the bladder after cyclophosphamide treatment for childhood acute lymphocytic leukemia. Pediatr Blood Cancer 42 (3): 289-91, 2004.
-
Frobisher C, Gurung PM, Leiper A, et al.: Risk of bladder tumours after childhood cancer: the British Childhood Cancer Survivor Study. BJU Int 106 (7): 1060-9, 2010.
Changes to This Summary (04 / 14 / 2017)The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above. Late Effects of the Cardiovascular System This section was comprehensively reviewed and extensively revised. Late Effects of the Endocrine System This section was comprehensively reviewed and extensively revised. Late Effects of the Reproductive System Added Table 14 about hazard ratios for the likelihood of reporting first pregnancy by cyclophosphamide equivalent dose for male and female survivors of childhood cancer. This summary is written and maintained by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® - NCI's Comprehensive Cancer Database pages. About This PDQ SummaryPurpose of This Summary This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the late effects of treatment for childhood cancer. It is intended as a resource to inform and assist clinicians who care for cancer patients. It does not provide formal guidelines or recommendations for making health care decisions. Reviewers and Updates This summary is reviewed regularly and updated as necessary by the PDQ Pediatric Treatment Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH). Board members review recently published articles each month to determine whether an article should: - be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary. The lead reviewers for Late Effects of Treatment for Childhood Cancer are: - Louis S. Constine, MD (James P. Wilmot Cancer Center at University of Rochester Medical Center)
- Melissa Maria Hudson, MD (St. Jude Children's Research Hospital)
- Nita Louise Seibel, MD (National Cancer Institute)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website's Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries. Levels of Evidence Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Pediatric Treatment Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations. Permission to Use This Summary PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary]." The preferred citation for this PDQ summary is: PDQ® Pediatric Treatment Editorial Board. PDQ Late Effects of Treatment for Childhood Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/childhood-cancers/late-effects-hp-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389273] Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images. Disclaimer Based on the strength of the available evidence, treatment options may be described as either "standard" or "under clinical evaluation." These classifications should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page. Contact Us More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's Email Us. Last Revised: 2017-04-14 Last modified on: 8 September 2017
|
|